Issue 4:1
Arteriovenous Graft Pseudoaneurysm
DOI: https://doi.org/10.21980/J8B06ZA bedside ultrasound of the mass demonstrated a large compressible hypoechoic structure (see purple outline) above the arteriovenous graft (see red outline). The contents demonstrated movement of fluid within the structure. This was confirmed with Doppler mode, which allowed for visualization of flow communicating between the structure and the underlying vessel, which is diagnostic for a pseudoaneurysm.
Bilateral Shoulder Dislocation after Ski Injury
DOI: https://doi.org/10.21980/J86929An anteroposterior chest X-ray demonstrates bilateral shoulder dislocations. Both the right and left humeral heads (blue lines) are displaced medially, anteriorly, and inferiorly from their normal positions in the glenoid fossae (red lines), thus signifying bilateral anterior dislocations. There is also a fracture of the left humeral head at the greater tubercle (green arrow).
Abdominal Pain with Black Tongue
DOI: https://doi.org/10.21980/J8XS7JPatient’s tongue had a black discoloration, without elongated filiform papillae. We could not appreciate lymphadenopathy. His abdomen was tender to palpation.
Beware the Devastating Outcome of a Common Procedure
DOI: https://doi.org/10.21980/J8T336Non-contrast head computed tomography (CT) demonstrates multifocal bilateral hypodense lesions (white arrows) representing air emboli. Note the lesions are located in the intra-axial distribution which indicates an underlying vascular origin.
Suspicious Skin Lesion in an 11-Year-Old Male
DOI: https://doi.org/10.21980/J8JK9TThe patient had a 5 cm ulcerative lesion with raised borders and a yellow, “fatty” center. There was no active drainage, site tenderness, or lymphadenopathy.
Guilty as Charged: Jailed Coronary Vessel Presenting as Wellens’ Syndrome Type B
DOI: https://doi.org/10.21980/J8DS6HEvolving changes to electrocardiograph (ECG) were noted during serial ECG monitoring involving leads V2 and V3, along with some T-wave inversion in V4 and V5 that were concerning for a Wellens’ syndrome type B on second ECG. She was admitted and subsequently taken to cardiac catheterization suite where it was revealed that the previously placed stent in the left anterior descending (LAD) artery was patent. Unfortunately, the stent blocked off an adjacent side branch vessel off the LAD in proximal two-third region of the stent (as seen in the cartoon).
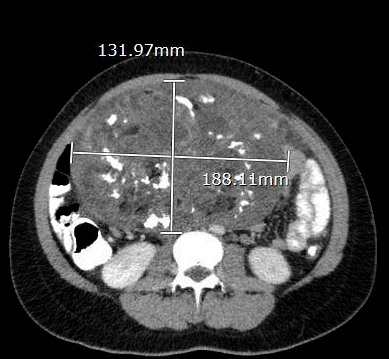
Ovarian Teratoma
DOI: https://doi.org/10.21980/J8934XThe CT scan with oral contrast in the emergency department revealed a large heterogeneous abdominopelvic mass measuring 13.2 x 18.8 x 23.1 cm (see white lines), suggestive of an ovarian teratoma from the right ovary. This mass included fat, fluid, calcifications (see yellow arrows), and enhancing soft tissue components. The teratoma resulted in mass effect upon large and small bowel loops (see blue highlighted areas), inferior vena cava (IVC), distal aorta (see red highlighted area) and right common iliac artery. A small volume of ascites was also observed. There was no evidence of bowel obstruction, vascular occlusion or other significant emergent finding. Additionally, transabdominal and transvaginal ultrasound images were obtained. The transabdominal image visualized the abdominopelvic mass (see four yellow stars). The transvaginal image visualized a cross section of the teratoma (see four red stars) in relation to the bladder (see four blue stars).
Warm & Blue: A Case of Methemoglobinemia
DOI: https://doi.org/10.21980/J8591MThe patient hadperioral cyanosis, blue coloration around her mouth, but the rest of the skin on her face appeared normal. She also had acrocyanosis to bilateral hands that can be seen in the image. The patient has a tan complexion up to the level of her wrists, but the palms of her hands are pale and cyanotic.