Hypopyon
History of present illness:
A 57-year-old male presented to the emergency department with left eye pain and progressively worsening vision for one month after being struck in the eye with a small piece of metal. At the time of the accident, the patient was seen by an ophthalmologist who prescribed eye drops and provided referral for a computed tomography scan of the orbits, which was not obtained.
Significant findings:
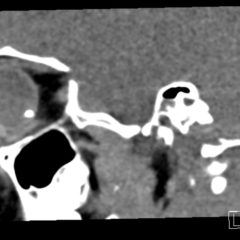
Physical examination of the left eye revealed a hypopyon (green arrow) – which is a layered white to yellow sediment in front of the inferior aspect of the iris associated with scleral injection and chemosis. Extraocular movements were intact bilaterally and pain did not worsen with extraocular movement. The pupil was poorly reactive to direct light and only hand movement could be perceived. The intraocular pressure was 14 mmHg. Slit lamp exam demonstrated a dense cataract. Bedside ocular ultrasound demonstrated vitreous opacities concerning for possible intraocular foreign bodies.
Discussion:
A hypopyon is an accumulation of leukocytes in the anterior chamber due to severe intraocular inflammation.1 Differential diagnoses include endophthalmitis, infectious corneal ulcer, severe iridocyclitis, retained intraocular foreign body, intraocular tumor necrosis, recurrent corneal erosion, drugs (eg, rifampin), leukemia and can be seen post cataract surgery – sterile or infected due to device contaminant.2 While a hypopyon can often be seen without magnification, a slit lamp examination is essential to adequately evaluate the anterior chamber for possible etiologies. Inflammation of the anterior chamber can be seen as cells and flare.3
Hypopyon is associated with nearly 85% cases of acute endophthalmitis and therefore warrants prompt ophthalmology consultation for surgical intervention and initiation of intravitreal antibiotics.4 Treatment upon discharge typically involves intensive topical steroids and topical antibiotics. Oral systemic antibiotics may also be considered as they may sometimes reach therapeutic vitreous levels.5 Topical atropine is often added to reduce ciliary spasm and minimize the development of synechiae or adhesions.6 Endophthalmitis is an ocular emergency that carries a poor visual prognosis if not treated aggressively.7
The patient in this case was started on broad spectrum intravenous antibiotics and taken emergently to the operating room by ophthalmology. He was diagnosed with endophthalmitis likely caused by the retained foreign body from the trauma four weeks prior. He had significant improvement in his vision following operative intervention. He was discharged home with antibiotics, atropine drops and close ophthalmology follow-up.
Topics:
Hypopyon, ophthalmology, ocular emergency, endophthalmitis, retained foreign body.
References:
- Mahmood AR, Narang AT. Diagnosis and management of the acute red eye. Emerg Med Clin North Am. 2008;26(1):35-55. doi: 10.1016/j.emc.2007.10.002
- Differential diagnosis of ocular signs. In: Bagheri N, Wajda BN, Calvo CM, Durrani AK, Friedberg MA, Rapuano CJ, eds. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 7th Philadelphia, PA: Wolters Kluwer; 2017:38.
- Robinett DA, Kahn JH. The physical examination of the eye. Emerg Med Clin North Am. 2008;26(1):1-16. doi: 10.1016/j.emc.2007.11.007
- Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113(12):1479-1496.doi: 10.1001/archpht.1995.01100120009001
- In: Bagheri N, Wajda BN, Calvo CM, Durrani AK, Friedberg MA, Rapuano CJ, eds. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 7thed. Philadelphia, PA: Wolters Kluwer; 2017:297.
- Ojaimi E, Wong DT. Endophthalmitis, prevention and treatment. In: Zaidi FH, ed. Cataract surgery. Croatia: InTech; 2013:S265-284.
- Guluma K, Lee JE. Ophthalmology. In: Walls RM, Hockberger RS, Gausche-Hill M, et al, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th Philadelphia, PA: Elsevier; 2018:790-819.e3.
- Nickson C. The aching red photophobic eye. Life in the Fast Lane. https://litfl.com/the-aching-red-photophobic-eye/. Updated October 26, 2018. Accessed November 8, 2018.