Search By Topic
Found 36 Unique Results
Page 1 of 4
Page 1 of 4
Page 1 of 4
A Simulation and Small-Group Pediatric Emergency Medicine Course for Generalist Healthcare Providers: Gastrointestinal and Nutrition Emergencies
DOI: https://doi.org/10.21980/J8WH2KThe aim of this curriculum is to increase learners’ proficiency in identifying and stabilizing acutely ill pediatric patients with gastrointestinal medical or surgical disease or complications of malnutrition. This module focuses on the diagnosis and management of gastroenteritis, acute bowel obstruction, and deficiencies of feeding and nutrition. The target audience for this curriculum is generalist physicians and nurses in limited-resource settings.
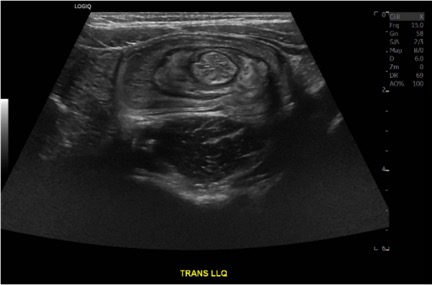
Case Report of a Child with Colocolic Intussusception with a Primary Lead Point
DOI: https://doi.org/10.21980/J8564QOn the initial ED visit, an abdominal ultrasound (US) was ordered which showed the classic intussusception finding of a target sign (yellow arrow), or concentric rings of telescoped bowel, on the transverse view of the left lower quadrant (LLQ).
Adolescent with Diabetic Ketoacidosis, Hypothermia and Pneumomediastinum
DOI: https://doi.org/10.21980/J8FP8JBy the end of the simulation, learners will be able to: 1) develop a differential diagnosis for an adolescent who presents obtunded with shortness of breath; 2) discuss the management of diabetic ketoacidosis; 3) discuss management of hypothermia in a pediatric patient; 4) discuss appropriate ventilator settings in a patient with diabetic ketoacidosis; and 5) demonstrate interpersonal communication with family, nursing, and consultants during high stress situations.
Little Patients, Big Tasks – A Pediatric Emergency Medicine Escape Room
DOI: https://doi.org/10.21980/J89W70By the end of this small group exercise, learners will be able to: 1) demonstrate appropriate dosing of pediatric code and resuscitation medications; 2) recognize normal pediatric vital signs by age; 3) demonstrate appropriate use of formulas to calculate pediatric equipment sizes and insertion depths; 4) recognize classic pediatric murmurs; 5) appropriately diagnose congenital cardiac conditions; 6) recognize abnormal pediatric electrocardiograms (ECGs); 7) identify life-threatening pediatric conditions; 8) demonstrate intraosseous line (IO) insertion on a pediatric model; and 9) demonstrate appropriate use of the Neonatal Resuscitation Protocol (NRP®) algorithms.
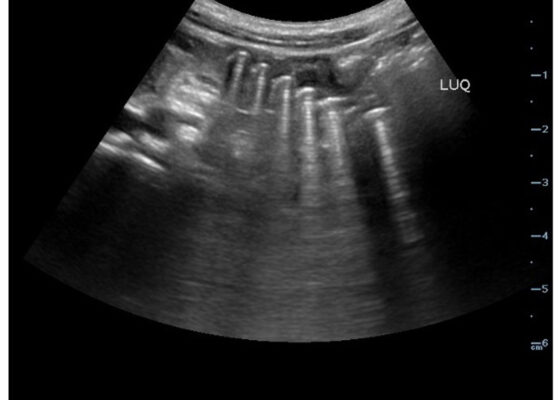
Point-Of-Care Ultrasound Use for Detection of Multiple Metallic Foreign Body Ingestion in the Pediatric Emergency Department: A Case Report
DOI: https://doi.org/10.21980/J83D2DBedside POCUS was performed on the patient’s abdomen using the curvilinear probe. The left upper quadrant POCUS image demonstrates multiple hyperechoic spherical objects with shadowing and reverberation artifacts concerning multiple foreign body ingestions. Though the patient and mother initially denied knowledge of foreign body ingestion, on repeated questioning after POCUS findings, the patient admitted to his mother that he ate the spherical magnets he received for his birthday about one week ago. The patient swallowed these over the course of two days. The presence of multiple radiopaque foreign bodies was confirmed with an abdominal X-ray.
Child Maltreatment Education: Utilizing an Escape Room Activity to Engage Learners on a Sensitive Topic
DOI: https://doi.org/10.21980/J84H1CBy the end of the escape room, the learner should be able to: 1) understand the national and local prevalence of child maltreatment; 2) understand the different types of child maltreatment and common associated presentations; 3) know the local EMS agency reporting requirements; 4) understand when to make base hospital contact with respect to concern for maltreatment; 5) collaborate effectively as a team.
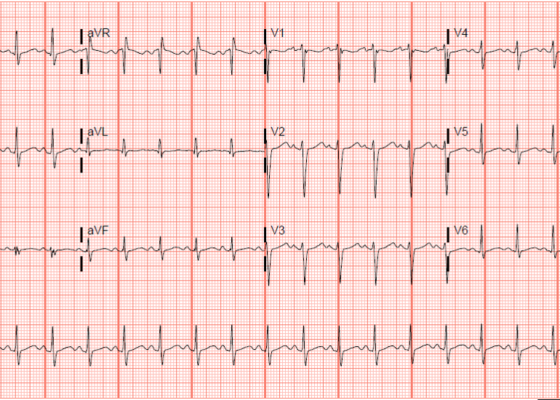
Electrocardiogram Abnormalities Following Diphenhydramine Ingestion: A Case Report
DOI: https://doi.org/10.21980/J85H1PThe blue arrow points to one of the terminal R waves in aVR, and the green arrow points to one of the large S waves in lead I, indicating right axis deviation. These findings are pathognomonic for sodium channel blockade. Due to the specific ECG findings and knowledge of diphenhydramine overdose, it was evident that these ECG findings were due to a cardiac sodium channel blockade. Sodium channels are essential within myocardial tissue to ensure the rapid upstroke of cardiac action potential, as well as rapid impulse conduction throughout cardiac tissue. Therefore, sodium channel blockers tend to exhibit significant dysrhythmic properties due to severe conduction disturbances.2 The blockage of the cardiac sodium channels appears as terminal R waves in aVR as well as terminal S waves in lead I due to delaying, and possibly blocking, the electrical conduction pathway of the heart. The orange arrows show resolution of terminal R wave in aVR and terminal S wave in lead I, after administration of sodium bicarbonate.
A Case of Community-Acquired Tuberculosis in an Infant Presenting with Pneumonia Refractory to Antibiotic Therapy
DOI: https://doi.org/10.21980/J8X07MChest radiographs during the initial presentation at seven weeks of life demonstrated right lower lobe (RLL) air space opacity on both PA and lateral views, compatible with pneumonia (referenced by yellow and green arrows, respectively). Repeat chest radiograph performed 12 days after the initial imaging revealed persistent right lower lobe opacity and right hilar fullness, seen as an opacified projection off of the mediastinal border as compared with the prior image, concerning for lymphadenopathy (designated by the aqua arrow). On the third presentation, computed tomography (CT) of the chest with intravenous contrast found persistent right lower lobe consolidation, innumerable 2-3 mm nodules, and surrounding ground glass opacities. This is best visualized as scattered areas of hyperdensity in the lung parenchyma. Axial images confirmed the presence of right hilar as well as subcarinal lymphadenopathy (indicated by white and pink arrows, respectively). Magnetic resonance imaging (MRI) of the brain with IV contrast was performed which showed a punctate focus of enhancement in the left precentral sulcus compatible with a tuberculoma (denoted with red arrow).
Respiratory Distress in the Pediatric ED: A Case-based Self-directed Learning Module
DOI: https://doi.org/10.21980/J8T64MEducational Objectives: By the end of this module, learners will be able to: 1) recognize the unique pathophysiology for respiratory distress in the pediatric population and formulate a broad differential; 2) understand the treatment principles for the most common causes of respiratory distress in children; 3) navigate and apply validated clinical decision-making tools for treatment of pediatric respiratory illnesses.
Infant Botulism
DOI: https://doi.org/10.21980/J8X35WAfter this simulation learners should be able to: 1) develop a differential diagnosis for the hypotonic infant, 2) recognize signs and symptoms of infant botulism, 3) recognize respiratory failure and secure the airway with appropriate rapid sequence intubation (RSI) medications, 4) initiate definitive treatment of infant botulism by mobilizing resources to obtain antitoxin, 5) continue supportive management and admit the patient to the pediatric intensive care unit (PICU), 6) understand the pathophysiology and epidemiology of infant botulism, 7) develop communication and leadership skills when evaluating and managing critically ill infants.