Search By Topic
Found 55 Unique Results
Page 1 of 6
Page 1 of 6
Page 1 of 6
Modification of an Airway Training Mannequin to Teach Engagement of the Hyoepiglottic Ligament
DOI: https://doi.org/10.21980/J8R06PBy the end of this education session, participants should be able to: 1) identify relevant airway anatomy during intubation, including base of the tongue, epiglottis, midline vallecular fold, anterior arytenoids; 2) appreciate the value of a stepwise anatomically guided approach to intubation; 3) become familiar with the midline vallecular fold and underlying anatomy, including the hyoepiglottic ligament, and how proper placement of the laryngoscope can result in improved glottic visualization.
Adolescent with Diabetic Ketoacidosis, Hypothermia and Pneumomediastinum
DOI: https://doi.org/10.21980/J8FP8JBy the end of the simulation, learners will be able to: 1) develop a differential diagnosis for an adolescent who presents obtunded with shortness of breath; 2) discuss the management of diabetic ketoacidosis; 3) discuss management of hypothermia in a pediatric patient; 4) discuss appropriate ventilator settings in a patient with diabetic ketoacidosis; and 5) demonstrate interpersonal communication with family, nursing, and consultants during high stress situations.
Inhalational Injury Secondary to House Fire
DOI: https://doi.org/10.21980/J8TW7NAt the conclusion of the simulation session, learners will be able to: 1) recognize the indications for intubation in a thermal burn/inhalation injury patient; 2) develop a systematic approach to an inhalational injury airway; and 3) recognize indications for transfer to burn center.
How to Build a Low-Cost Video-Assisted Laryngoscopy Suite for Airway Management Training
DOI: https://doi.org/10.21980/J8C068Using an anatomically accurate airway simulator, by the end of a 20–30-minute instructional session, learners should be able to: 1) Understand proper positioning and use the video laryngoscope with dexterity, 2) identify airway landmarks via the video screen, and 3) demonstrate ability to intubate a simulated airway.
Acute Exacerbation of COPD
DOI: https://doi.org/10.21980/J8V070By the end of this simulation, learners will be able to (1) assess for causes of severe shortness of breath, (2) manage severe COPD exacerbation by administering appropriate medications, (3) identify worsening clinical status and initiate NIPPV, (4) assess the causes of hypoxia after establishing endotracheal intubation and, (5) identify indication for needle decompression and perform chest tube thoracostomy.
Telemedicine Consult for Shortness of Breath Due to Sympathetic Crashing Acute Pulmonary Edema
DOI: https://doi.org/10.21980/J8HS86At the completion of the simulation and debriefing, the learner will be able to: 1) recognize the physical exam findings and presentation of SCAPE, 2) utilize imaging and laboratory results to further aid in the diagnosis of SCAPE, 3) initiate treatments necessary for the stabilization of SCAPE, 4) demonstrate the ability to assist with the stabilization and disposition of a patient via tele-medicine as determined by the critical action checklist and assessment tool below, 5) interpret the electrocardiogram (EKG) as atrial fibrillation with rapid ventricular response (AFRVR), and 6) recognize that SCAPE is the underlying cause of AFRVR and continue to treat the former.
Electronic Cigarette or Vaping-Associated Lung Injury Case Report
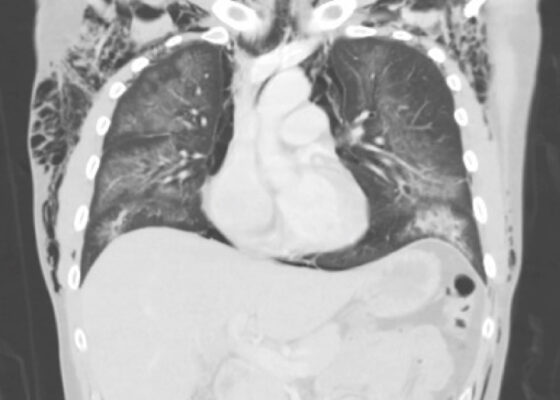
DOI: https://doi.org/10.21980/J8S65PThe CT of the chest with contrast showed subcutaneous emphysema (green star), pneumomediastinum (yellow arrow), and pneumopericardium (purple asterix) without an identifiable tracheal tear. Extensive air was visualized as hypodense areas within the chest wall within the soft tissue. The image also detailed a hypodense area surrounding the heart consistent with pneumopericardium. No disruption of the trachea was present. Additionally, the CT of the chest also showed bilateral ground glass airspace opacities (red stars) with subpleural sparing that is consistent with EVALI findings.2,5 These specific findings have been seen in many of the EVALI cases.5 This image is interesting because there is extensive pneumomediastinum with no clearly identifiable cause. The imaging shows no esophageal or tracheal or lung injury, so it is important to note relevant information collected during interview regarding patient’s recent history of vaping THC, especially when establishing a differential diagnosis.
Respiratory Distress in the Pediatric ED: A Case-based Self-directed Learning Module
DOI: https://doi.org/10.21980/J8T64MEducational Objectives: By the end of this module, learners will be able to: 1) recognize the unique pathophysiology for respiratory distress in the pediatric population and formulate a broad differential; 2) understand the treatment principles for the most common causes of respiratory distress in children; 3) navigate and apply validated clinical decision-making tools for treatment of pediatric respiratory illnesses.
Zombie Cruise Ship Virtual Escape Room for POCUS Pulmonary: Scan Your Way Out
DOI: https://doi.org/10.21980/J8RM0MBy the end of performing the Zombie Cruise Ship Virtual Escape Room, learners will be able to: 1) recognize sonographic signs of A-line, B-line, Barcode sign, Bat sign, Seashore Sign, Plankton sign, Jellyfish Sign, Lung point, lung lockets, and Lung pulse; 2) differentiate sonographic findings of pneumothorax, hemothorax, pneumonia, COVID 19 pneumonia, pulmonary edema, and pleural effusion from normal lung findings; 3) distinguish pneumonia from atelectasis by recognizing dynamic air bronchogram; and 4) recognize indications for performing POCUS pulmonary such as dyspnea, blunt trauma, fall, cough and/or heart failure.
Case Report of an Empyema Identified on Lung Ultrasound
DOI: https://doi.org/10.21980/J8SH2NUsing a curvilinear ultrasound probe, images of the patient were obtained from the left mix-axillary line. These images demonstrate a loculated left-sided pleural effusion (outlined in the attached ultrasound image in blue) that was moderate in size, concerning for an empyema. The diaphragm on the right (red) of the image outlines the inferior margin of the collection of pus, which is seen in the inferior aspect of the left lung. Unfortunately, rib shadows on the left side of the image prevent the full empyema from being captured in this single image. As a result of the bedside ultrasound, however, the patient was rapidly diagnosed with an empyema and was initiated on antibiotics, which is further discussed below. After his bedside ultrasound was completed, his chest x-ray revealed the expected left-sided pleural effusion. Additionally, a CT angiogram of the chest was ordered to rule out a pulmonary embolism, which was negative for an embolism but does redemonstrate the left-sided loculated pleural effusion (outlined on the CT axial and coronal images in blue).