Guilty as Charged: Jailed Coronary Vessel Presenting as Wellens’ Syndrome Type B
History of present illness:
A 44-year-old Caucasian female with moderate-risk factors for cardiovascular event presented to the emergency department (ED) complaining of acute chest pain. She was diagnosed with myocardial infarction and had a percutaneous coronary angiography stent placed in the circumflex coronary artery. She was discharged home two days later.
The patient returned to the ED eight days after discharge for non-symptomatic elevated blood pressure. In consultation with her cardiologist, she was discharged home from the ED the same day after brief observation and non-revealing workup. The patient returned to the ED, for her third visit in fourteen days, with a nonspecific complaint of fatigue, weakness, and low level, intermittent, non-localized chest discomfort. The work-up in the ED revealed a minor increase in her baseline troponin that was below threshold for concerning myocardial tissue damage.
Significant findings:
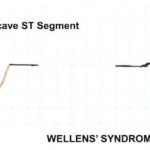
Evolving changes to electrocardiograph (ECG) were noted during serial ECG monitoring involving leads V2 and V3, along with some T-wave inversion in V4 and V5 that were concerning for a Wellens’ syndrome type B on second ECG. She was admitted and subsequently taken to cardiac catheterization suite where it was revealed that the previously placed stent in the left anterior descending (LAD) artery was patent. Unfortunately, the stent blocked off an adjacent side branch vessel off the LAD in proximal two-third region of the stent (as seen in the cartoon).
Wellens’ syndrome is associated with specific characteristic T-wave changes on ECG in leads V1, V2, and V3 in asymptomatic individuals, or in those with intermittent or non-specific chest discomfort as was in our case.1 There are two T-wave characteristic changes associated with Wellens’ syndrome, namely type A and B: type B, a deep inverted T-wave in V2 and V3 as was seen in our case; and type A, a biphasic T-wave in V2 and V3.2,3 A slight ST depression may also be observed in V1, especially in individuals presenting with chest discomfort. These changes are thought to result from reperfusion of stenosis in the LAD artery and therefore require prompt treatment.4 There is a proposed 75% probability of an acute myocardial infarction in type A, and 25% in type B within one week of discovery if not addressed promptly.1,5
Discussion:
To our knowledge, this is the first documented case of a jailed coronary stent presenting as a Wellens’ syndrome. Wellens’ syndrome is well described in the literature as an ECG change consistent with critical stenosis of the LAD and a probable precursor lesion of an acute myocardial infarction.2,4
There were very few documented cases of jailed stents following coronary stent placement or its management in the literature.6,7,8 Treatment of a jailed stent involves insertion of a guidewire into the jailed branch to dilate its ostium.9,10 Bhargava et al. studied the implications of jailed stents following coronary stent placement and suggested that the structure of NIR stents lessen both clinical and functional significance of a jailed stent.6 Contrary to our perception of an acute re-stenosis of the stented vessel upon observation of the ECG changes, the angiography performed revealed an adjacent jailed diagonal branch of the LAD artery in the proximal two-third area of the previously placed stent. Consistent with the literature review, the jailed vessel in our case was not clinically significant. An interesting correlation in the body of evidence to findings in our case was that the patient’s post-stent angiography showed a global improvement in coronary blood flow as compared to pre-stent placement status.
Immediate treatment was initiated in ED and followed promptly by the cardiovascular team. Although the patient presentation was vague and nonspecific, the emergency physician’s recognition of Wellens’ syndrome led to timely return to cardiac the catheterization suite, accurate diagnosis, and optimum management in a seamless manner, with good patient outcome. The cardiovascular team concluded that the jailed vessel was not amenable to invasive intervention but optimized her medical management due to functional impairment.
The patient underwent a six-minute-walk test with reassuring results of a good response to medical optimization without further complication as of the time of this writing. While a rescue intervention was not possible in this case, there are few documented cases where minimal intervention is possible to rescue jailed coronary vessels.6
In conclusion, we presented a unique case of Wellens’ syndrome resulting from coronary stent placement. While it rarely occurs, we would like to remind ED physicians to be aware of this phenomenon particularly when caring for patients who are at higher risk of coronary events that present with non-specific complaints. As emergency physicians, we should remind ourselves of Wellens’ syndrome criteria and utilize this knowledge to efficiently manage and activate essential resources to prevent impending or expansion of myocardial tissue damage, thereby improving patient outcome.
Topics:
Jailed vessel, Wellens’ Syndrome types A and B, ECG changes.
References:
- Movahed MR. Wellens’ syndrome or inverted U-waves? Clin Cardiol. 2008;31(3):133-134. doi: 10.1002/clc.20222.
- Grautoff S. Wellens’ syndrome can indicate high-grade LAD stenosis in case of left bundle branch block. Herzschrittmachertherapie & Elektrophysiol. 2017;28(1):57. doi: 10.1007/s00399-017-0489-z
- Sobnosky S, Kohli R, Bleibel S. Wellens’ syndrome. The Internet Journal of Cardiology. 2005;3(1):1-4.
- De Zwaan C, Bar FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4 Pt 2):730-736.
- Mead NE, O’Keefe KP. Wellen’s syndrome: an ominous EKG pattern. J Emerg Trauma Shock. 2009; 2(3):206–208. doi: 10.4103/0974-2700.55347
- Bhargava B, Waksman R, Lansky AJ, Kornowski R, Mehran R, Leon MB. Clinical outcomes of compromised side branch (stent jail) after coronary stenting with the NIR stent. Catheter Cardiovasc Interv. 2001;54(3):295-300.
- Koo BK, Waseda K, Kang HJ, et al. Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010;3(2):113-119. doi: 10.1161/CIRCINTERVENTIONS.109.887406
- Ahn JM, Lee JY, Kang SJ, et al. Functional assessment of jailed side branches in coronary bifurcation lesions using fractional flow reserve. JACC: Cardiovascular Interventions. 2012;5(2):155-161; doi: 10.1016/j.jcin.2011.10.015
- Caputo RP, Chafizadeh ER, Stoler RC, et al. Stent jail: a minimum-security prison. Am J Cardiol. 1996;77(14):1226-1229.
- Koo BK, Kang HJ, Youn TJ, et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46(4):633-637. doi: 10.1016/j.jacc.2005.04.054