X-Ray
Case Report: Traumatic Tension Pneumothorax in a Pediatric Patient
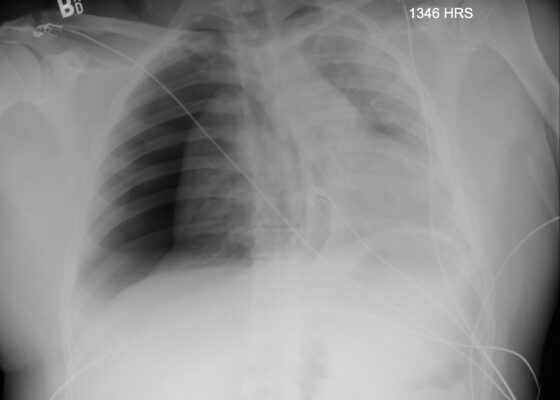
DOI: https://doi.org/10.21980/J8ZD1SChest X-ray demonstrated significant right-sided pneumothorax (with red outline showing border of collapsed right lung) with cardio mediastinal shift to the left (shown by blue arrows) indicative of a tension pneumothorax
Adult Clavicular Fracture Case Report
DOI: https://doi.org/10.21980/J8FM0TThe patient's chest and clavicular radiographs showed a comminuted displaced acute fracture of the right mid-clavicle (green, blue, yellow). The clavicular fracture was also visible on the chest computed tomography (CT). The remainder of his trauma workup was negative for acute findings.
Case Report of Distal Radioulnar Joint and Posterior Elbow Dislocation
DOI: https://doi.org/10.21980/J89S6KRadiographs of the left elbow and wrist were obtained. Left elbow radiographs showed simple posterolateral dislocation of the olecranon (red) without fracture of the olecranon (red) or trochlea (blue). Left wrist lateral radiographs demonstrated DRUJ dislocation with dorsal displacement of the distal ulna (green) without fracture or widening of the radioulnar joint (purple). Post-reduction radiographs demonstrated appropriate alignment of the elbow with the trochlea seated in the olecranon and improved alignment of the DRUJ.
A Case Report of Ogilvie’s Syndrome in a 58-year-old Quadriplegic
DOI: https://doi.org/10.21980/J82922Plain radiograph of the patient's abdomen revealed a gaseous distention of the colon. This is demonstrated as noted in the abdominal x-ray as gaseous distention, most notably in the large bowel (arrows) including the rectal region (large circle). Follow up computed tomography (CT) scan affirmed severe pancolonic gaseous distention measuring up to 11.2 cm, compatible with colonic pseudo-obstruction as noted by the large red arrows. No anatomical lesion or mechanical obstruction was observed, as well as no evidence of malignancy or other acute process.
Is an X-ray a Useful Test for Esophageal Food Boluses? A Case Report
DOI: https://doi.org/10.21980/J8Q639The plain film radiograph of the chest demonstrated a fluid level (yellow arrow) in the distal esophagus with dilation of the esophagus proximal to that point (blue line). Neither of these findings were present on the previous visit.
Case Report: Talar Neck Fracture
DOI: https://doi.org/10.21980/J8FP75ABSTRACT: This report demonstrates a case of a severe talar neck fracture. Although rare, talar neck fractures have a high potential for morbidity. Typically caused by a high energy injury, this patient’s mechanism of injury was relatively minor, and presentation was not immediately concerning for such a severe fracture. Initial x-rays provided a gross demonstration of the fracture, but a
A Case Report on Miliary Tuberculosis in Acute Immune Reconstitution Inflammatory Syndrome
DOI: https://doi.org/10.21980/J81H02A portable single-view radiograph of the chest was obtained upon the patient’s arrival to the ED resuscitation bay that showed diffuse reticulonodular airspace opacities (red arrows) seen throughout the bilateral lungs, concerning for disseminated pulmonary tuberculosis. Subsequently, a computed tomography (CT) angiography of the chest was obtained which again demonstrates this diffuse reticulonodular airspace opacity pattern (red arrows).
Case Report of Untreated Pediatric Femoral Neck Fracture with Osteopenia
DOI: https://doi.org/10.21980/J8S92KOn her right hip radiograph, the patient was found to have a right femoral neck fracture with superior displacement of the intertrochanteric portion of the right femur. Moreover, the radiograph demonstrated diffuse osteopenia of the right hip and femur from chronic disuse as characterized by the increased radiolucency of the cortical bones compared to the left side.