Ultrasound
Point-of-care Ultrasound in the Diagnosis and Monitoring of Bladder Hematoma vs. Hemorrhage
DOI: https://doi.org/10.21980/J8092FBladder POCUS demonstrated 500mL of post void residual fluid, indicative of retention. Half of the volume is hyperechoic (red circle); this is likely the bladder wall hematoma. Could also consider sonographic artifact, bladder mass, or cystitis.1-2
Point-of-Care Ultrasound to Evaluate Intrahepatic Biliary Stent Function
DOI: https://doi.org/10.21980/J86S6NThe ultrasound image demonstrates severe intrahepatic biliary ductal dilatation without an obvious intrahepatic obstructive lesion, as pointed out by the white arrows. The hepatic vasculature is well-distinguished from the biliary tree via color flow doppler, as seen by the white arrowheads.
Diagnosis and Treatment of an Anterior Shoulder Dislocation with Bedside Ultrasound
DOI: https://doi.org/10.21980/J8Z924Bedside ultrasound with the transducer placed on the posterior right shoulder revealed an anterior dislocation of the right humerus. This is evident by displacement of the humeral head further away from the posteriorly placed ultrasound transducer, and appears deep to the glenoid cavity. In a posterior shoulder dislocation, the humeral head would appear closer to the transducer (and the near field of the ultrasound image) than the glenoid. Note that a hypoechoic, heterogeneous fluid collection is within the joint space, compatible with a hematoma. A right shoulder X-ray confirmed the anterior dislocation with no evidence of fracture. Under direct ultrasound guidance the glenohumeral joint space was injected with 10 mL of 2% lidocaine as an intraarticular anesthetic block. The right shoulder was reduced using continual traction. Post-reduction ultrasound demonstrated a successful shoulder reduction, depicted by the humeral head being relocated to its anatomical location, adjacent to the glenoid cavity, as noted on the ultrasound image. A hematoma remains present within the joint space. Successful shoulder reduction was further confirmed by X-ray. The patient’s arm was placed in a sling and she was discharged home with orthopedics follow-up.
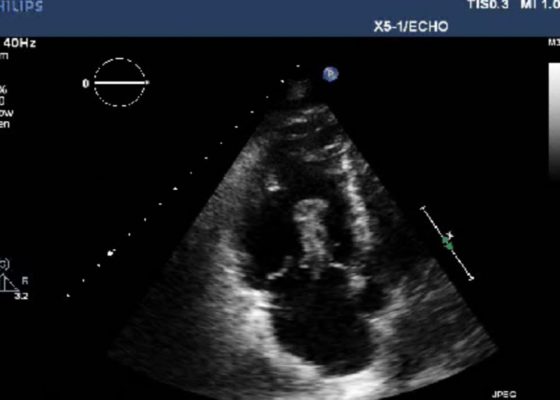
Right Atrial Thrombus
DOI: https://doi.org/10.21980/J8F93V History of present illness: A 77-year-old male presented to the emergency department with shortness of breath. Symptoms progressively worsened over the last 4-5 days, and on arrival was associated with chest tightness. He denied any medical conditions, smoking, or pertinent family history. He has not seen a primary care physician in “many years.” Upon arrival he was in mild
Posterior Vitreous Detachment
DOI: https://doi.org/10.21980/J89K9NOcular ultrasound was performed and demonstrated a thin, slightly echogenic strand (blue arrow) extending from the posterior eye into the vitreous humor (yellow arrow) which was hyperkinetic with extraocular motion. These findings are consistent with a posterior vitreous detachment (PVD).
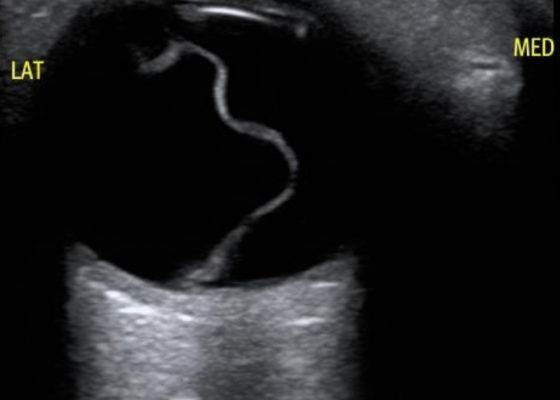
Macula-Off Retinal Detachment Identified on Bedside Ultrasound
DOI: https://doi.org/10.21980/J8WP8KPoint-of-care ultrasound was performed, demonstratinga free-floating, serpiginous, hyperechoic membrane (R) tethered at the optic nerve (ON) and ora serrata (OS), but detached at the macula (M) lateral to the optic nerve. This is diagnostic for macula-off retinal detachment. It can be differentiated from macula-on retinal detachment, in which the hyperechoic retina would appear attached posteriorly at the location of the macula just lateral to the optic nerve. Ophthalmology was consulted, agreed with the diagnosis of macula-off retinal detachment, and took the patient to the OR for laser photocoagulation.
Point-of-Care Ultrasound for the Diagnosis of Systolic Heart Failure
DOI: https://doi.org/10.21980/J8HD1RBedside ultrasound with the phased array probe was used to obtain a parasternal long axis view which demonstrated poor contractility and a severely decreased ejection fraction (EF). M-mode was placed over the anterior leaflet of the mitral valve to create a tracing depicting both the E-wave of early diastole (green arrow) and the A-wave from the atrial kick (blue arrow). The shortest distance between the septum and the mitral valve on the M-mode tracing gives the patient’s E-Point Septal Separation (EPSS) (pink arrow). EF can be estimated using the formula EF=75.5-2.5 x EPSS (in mm). This patient’s EPSS was measured to be 20mm which estimates that she had an EF of 25.5%.
Bedside Ultrasound for the Rapid Diagnosis of Fournier’s Gangrene
DOI: https://doi.org/10.21980/J8CP99Point of care ultrasound (POCUS) utilizing a high-frequency linear probe revealed heterogeneous debris with subcutaneous air within the scrotal wall extending into the perineum consistent with necrotizing fasciitis of the perineum or Fournier’s gangrene (FG). The video shows multiple foci of gas that appear as echogenic dots with “dirty shadows” posteriorly from reverberation artifact arising from gas within the soft tissue.