Brief Review of Intussusception Diagnosis and Management
History of present illness:
A 6-year-old male presented to the emergency department (ED) with acute onset of abdominal pain and multiple episodes of vomiting and diarrhea after his lunch at school. The patient’s mother was unsure if he had a fever. His sister had similar symptoms recently. Upon arrival, the patient was hypertensive, tachycardic and afebrile. He was drowsy but arousable. His abdomen was soft, with tenderness in the left lower quadrant. Laboratory findings showed leukocytosis of 18.1 x 1000/mm3. While in the ED, the patient developed a fever to 38.2°C.
Significant findings:
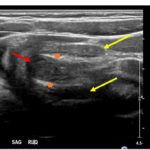
The patient’s abdominal ultrasound revealed intussusception in the right upper abdominal quadrant. The transverse ultrasound view showed a “doughnut sign” (dashed yellow line), telescoping bowel (yellow arrow), and invaginated hyperechoic mesenteric fat with crescent configuration (dashed orange line). The sagittal ultrasound view demonstrated the intussusception formed by the outer recipient bowel loop (yellow arrows), invaginated hyperechoic mesenteric fat (orange asterisks), and telescoping bowel centrally (red arrow).
Discussion:
Intussusception is an emergent condition in which a portion of bowel invaginates into a distal part of the intestine. It most commonly affects children aged 3 months to 3 years and is often preceded by a viral prodrome. Ninety percent of intussusception cases occur at the ileocolic junction where prominent lymphoid tissue acts as a lead point. Other possible lead points may include a Meckel’s diverticulum, polyp, appendicitis, or lymphoma.1
Many children with intussusception do not present with the classic triad of currant jelly stools, colicky abdominal pain, and vomiting. Intermittent abdominal pain is present in 80%-95% of patients, and bloody stools are present in only 50%-70% of cases. Patients may also present with lethargy, diarrhea, or septic shock if perforation or necrosis of bowel has occurred. Some studies suggest that clinical presentation varies by age with emesis, bloody stool, irritability, and lethargy more common in children less than 12 months old. Children greater than twelve months old were more likely to present with tenderness to palpation of the abdomen or abdominal pain.2 A delay in diagnosis can result in bowel ischemia, perforation, and increased need for surgical intervention.3 Therefore, it is crucial to maintain a high index of suspicion for intussusception in children presenting with any of the above symptoms.
Ultrasonography should be the initial imaging modality in cases with clinical suspicion for intussusception.4 Previously, contrast enemas were often used as a diagnostic tool and treatment modality. Studies have demonstrated that the modality choice had been related to age, with infants less than six months more likely to undergo enema while children greater than four were more likely to have a computed tomography scan or ultrasound.5 In the pediatric population, ultrasound has a sensitivity of 97.9% and specificity of 97.8% for diagnosis of ileocolic intussusception.6 A “doughnut,” “pseudokidney,” or “target sign” are diagnostic findings.3,7 The study could be performed by radiology or at the bedside in the ED.8,9 A study reported that with limited training, ED physicians could accurately perform ultrasound to diagnose intussusception, with a sensitivity of 85% and a specificity of 97%. Further studies are needed to determine the utility of bedside ultrasound for the diagnosis of intussusception in the community setting.3
Treatment in a stable, well-appearing child includes intravenous hydration and pediatric surgery consultation. The mainstay of non-operative therapy is air enema, often done under fluoroscopy, which has a success rate of approximately 90%.1 Occasionally, the bowel will reduce spontaneously without any intervention. If air enema fails, repeat air enema or surgical intervention is required. Other indications for surgery include hemodynamic instability, bowel necrosis, bowel perforation, or peritonitis.
This patient was transferred to a children’s hospital from which he was discharged home the next day. His two-week followed up document noted that the patient did not undergo any interventions, suggesting that his intussusception reduced spontaneously.
Topics:
Ultrasound, intussusception, gastrointestinal, point-of-care ultrasound (POCUS).
References:
- Charles T, Penninga L, Reurings JC, Berry MC. Intussusception in children: a clinical review. Acta Chir Belg. 2015; 115:5:327-333. doi: 10.1080/00015458.2015.11681124
- Mandeville K, Chien M, Willyerd FA, Mandell G, Hostetler MA, Bulloch B. Intussusception. Pediatr Emerg Care. 2012;28(9):842-844. doi: 10.1097/pec.0b013e318267a75e
- Riera A, Hsiao AL, Langhan ML, Goodman TR, Chen L. Diagnosis of intussusception by physician novice sonographers in the emergency department. Ann Emerg Med. 2012;60(3):264-268. doi:10.1016/j.annemergmed.2012.02.007
- Bartocci M, Fabrizi G, Valente I, Manzoni C, Speca S, Bonomo L. Intussusception in childhood: role of sonography on diagnosis and treatment. J Ultrasound. 2014;18(3):205-211. doi: 10.1007/s40477-014-0110-9
- Shekherdimian S, Lee SL. Management of pediatric intussusception in general hospitals: diagnosis, treatment, and differences based on age. World J Pediatr. 2010;7(1):70-73. doi: 10.1007/s12519-011-0249-9
- Hrychorczuk AL, Strouse PJ. Validation of US as a first-line diagnostic test for assessment of pediatric ileocolic intussusception. Pediatr Radiol. 2009;39(10):1075-1079. doi: 10.1007/s00247-009-1353-z
- Applegate K. Intussusception in children: evidence-based diagnosis and treatment. Pediatr Radiol. 2009;39(suppl 2): S140-S143. doi: 10.1007/s00247-009-1178-9
- Kairam N, Kaiafiss C, Shih R. Diagnosis of pediatric intussusception by an emergency physician-performed bedside ultrasound. Pediatri Emerg Care.2009;25(3):177-80. doi: 10.1097/PEC.0b013e31819a8a46
- Ramsey KW, Halm BM. Diagnosis of intussusception using bedside ultrasound by a pediatric resident in the emergency department. Hawaii J Med Public Health. 2014;73(2):58-60.