Arteriovenous Graft Pseudoaneurysm
History of present illness:
A 59-year-old male with a history of end stage renal disease on hemodialysis was sent to the emergency department (ED) by his dialysis center for concern for left upper extremity graft infection. The patient denied pain, fever, chills, or redness at the site. He did note a mass with a pustule at the fistula site that started that day, but there was no active drainage.
In the ED, the patient was well appearing, afebrile, with a normal heart rate and in no distress. Examination of the left upper extremity revealed a 1 cm mass with a sub centimeter discoloration of the overlying skin at the active fistula site. There was a palpable thrill and audible bruit.
Significant findings:
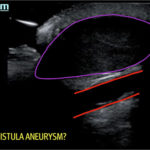
A bedside ultrasound of the mass demonstrated a large compressible hypoechoic structure (see purple outline) above the arteriovenous graft (see red outline). The contents demonstrated movement of fluid within the structure. This was confirmed with Doppler mode, which allowed for visualization of flow communicating between the structure and the underlying vessel, which is diagnostic for a pseudoaneurysm.
Discussion:
Vascular access (VA) complications involving either arteriovenous graft (AVG) or arteriovenous fistula (AVF) represent 36%-39%of hospitalizations in hemodialysis patients.1,2 Major complications include stenosis, thrombosis, infection, congestive heart failure, ischemic neuropathy, steal syndrome, and aneurysm. VA associated aneurysms can be divided into two groups: true and pseudoaneurysms. True aneurysms, which involve all layers of the vessel wall, are seen most often with AVFs and are mostly asymptomatic. In contrast, pseudoaneurysms occur outside the vessel wall due to a communicating defect in the graft. They are essentially hematoma encapsulated in adventitia that are prone to rupture.
Pseudoaneurysms are a relatively rare complication of vascular access with an incidence of 2%-10%.3 They often result from weakening of the vessel wall secondary to inflammation from infection or chronic needling which leads to scarring.4 Concerning signs that warrant vascular surgery consultation include an aneurysm that is symptomatic, twice the size of the graft, expanding, threatened viability of overlying skin, or large/multiple aneurysms limiting number of cannulation sites.5 Doppler ultrasound is the principal means of diagnosis with a sensitivity of 94%.6 On ultrasound there are several characteristic findings that can alert the provider to the diagnosis of pseudoaneurysm. On color doppler, visualization of a communication between the vessel and fluid collection external to the vessel is diagnostic.7 This connection is classically described as the yin-yang sign.7 Spectral doppler can demonstrate biphasic flow through the communication.7
The patient discussed here was seen by vascular surgery and admitted for surgical evaluation. After further records were obtained, the patient was found to have a history of three prior surgically removed pseudoaneurysms. Ultimately, he had ligation and excision of the graft two days later revealing two pulsatile pseudoaneurysms along the mid graft. The graft was unable to be salvaged, and he was scheduled for creation of a new fistula in the right arm.
Key points that guide the management of this case are the identification of changes overlying the fistula in the acute setting, prompting the use of bedside ultrasound, and necessitating vascular consultation. Any mass concerning for infection near a fistula or graft site should make a physician wary of possible aneurysm.
Topics:
Arteriovenous graft pseudoaneurysm, graft infection, dialysis complication, vascular access.
References:
- Rayner HC, Pisoni RL, Bommer J, et al. Mortality and hospitalization in haemodialysis patients in five European countries: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2004;19(1):108-120.
- Arora P, Kausz AT, Obrador GT, et al. Hospital utilization among chronic dialysis patients. J Am Soc Nephrol. 2000;11(4):740-746.
- Yasim A, Kabalci M, Eroglu E, Zencirci B. Complication of hemodialysis graft: anastomotic pseudoaneurysm: a case report. Transplant Proc. 2006;38(9):2816-2818. doi: 10.1016/j.transproceed.2006.08.099
- Mudoni A, Cornacchiari M, Gallieni M, et al. Aneurysms and pseudoaneurysms in dialysis access. Clinical Kidney Journal. 2015;8(4):363–367. doi: 10.1093/ckj/sfv042
- Jindal K, Chan CT, Deziel C, et al. Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology. J Am Soc Nephrol. 2006;17(3 Suppl 1):S1-S27. doi: 1681/ASN.2005121372
- Coughlin BF, Paushter DM. Peripheral pseudoaneurysms: evaluation with duplex US. Radiology. 1988;168(2):339–342. doi: 10.1148/radiology.168.2.3293107
- Davison BD, Polak JF. Arterial injuries: a sonographic approach. Radiol Clin N Am. 2004; 42:383–396. doi: 10.1016/j.rcl.2004.01.007