Ultrasound
Vaginal Bleeding Due to Iatrogenic Uterine Perforation – A Case Report
DOI: https://doi.org/10.21980/J83643The bedside transabdominal US of the pelvis showed a heterogeneous mixture of hypoechoic and hyperechoic endometrial thickening extending to the lower uterine segment (blue arrow), which was thought to represent active hemorrhage. Computed tomography of the abdomen and pelvis showed evidence of a large amount of endometrial hyperdensity (red arrow) suggestive of hemorrhagic contents within a grossly enlarged uterus. There was relative decreased enhancement of the uterine body and fundus, concerning for devascularization. There was also active extravasation along the left lateral uterus (yellow arrow).
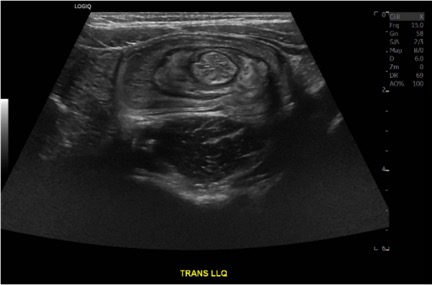
Case Report of a Child with Colocolic Intussusception with a Primary Lead Point
DOI: https://doi.org/10.21980/J8564QOn the initial ED visit, an abdominal ultrasound (US) was ordered which showed the classic intussusception finding of a target sign (yellow arrow), or concentric rings of telescoped bowel, on the transverse view of the left lower quadrant (LLQ).
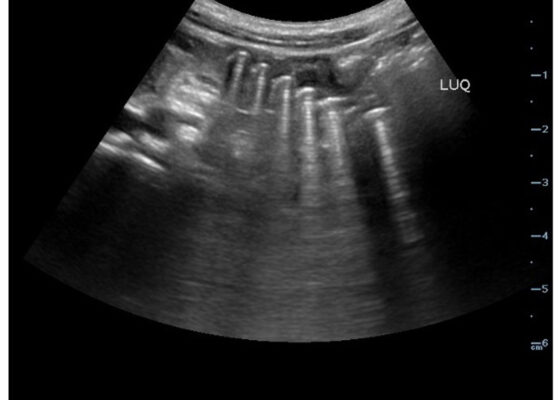
Point-Of-Care Ultrasound Use for Detection of Multiple Metallic Foreign Body Ingestion in the Pediatric Emergency Department: A Case Report
DOI: https://doi.org/10.21980/J83D2DBedside POCUS was performed on the patient’s abdomen using the curvilinear probe. The left upper quadrant POCUS image demonstrates multiple hyperechoic spherical objects with shadowing and reverberation artifacts concerning multiple foreign body ingestions. Though the patient and mother initially denied knowledge of foreign body ingestion, on repeated questioning after POCUS findings, the patient admitted to his mother that he ate the spherical magnets he received for his birthday about one week ago. The patient swallowed these over the course of two days. The presence of multiple radiopaque foreign bodies was confirmed with an abdominal X-ray.
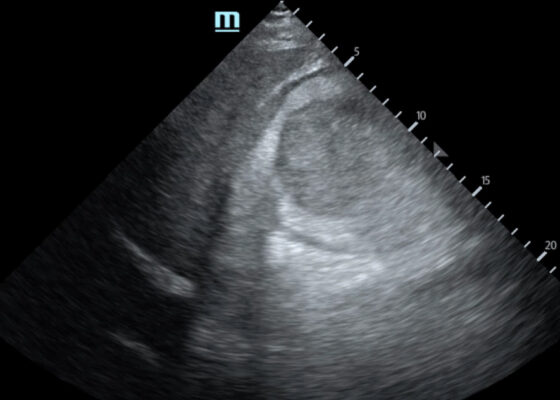
Sonographic Retrobulbar Spot Sign in Diagnosis of Central Retinal Artery Occlusion: A Case Report
DOI: https://doi.org/10.21980/J8735PThe bedside ocular ultrasound (B-scan) was significant for small, hyperechoic signal (white arrow) in the distal aspect of the optic nerve, concerning for embolus in the central retinal artery. Subsequent direct fundoscopic exam was significant for a pale macula with cherry red spot (black arrow), consistent with central retinal artery occlusion (CRAO).
Trauma by Couch: A Case Report of a Massive Traumatic Retroperitoneal Hematoma
DOI: https://doi.org/10.21980/J84D2QUpon arrival at the trauma center, a FAST revealed a large, well-circumscribed abnormality (red outline) deep to the liver (blue outline and star) and gallbladder (green outline and star). The right kidney and hepatorenal space were not clearly visualized. The remainder of the FAST showed no free fluid in the splenorenal space, pelvis, and no pericardial effusion. He had lung sliding bilaterally.
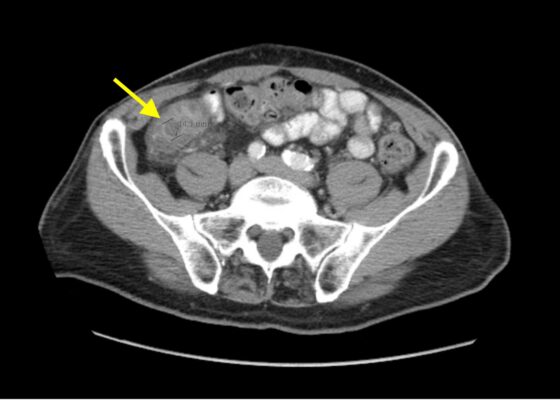
Imaging Findings of Small Bowel – Diverticulitis: A Case Report
DOI: https://doi.org/10.21980/J8F078Bedside ultrasound was performed and showed thickened bowel wall (orange marker), fat enhancement (green marker), and phlegmonous structure with central echogenicity (yellow marker). Imaging of the abdomen and pelvis with CT showed marked wall thickening and inflammatory change involving a 7.0cm segment of the distal/terminal ileum suspicious for severe ileitis with phlegmon and microabscess on the coronal image (yellow arrow). Additonally, the transverse images show a small rim-enhancing focus within this region of inflammation measuring up to 1.4cm which could represent microabscess (yellow arrow). Diagnosis of diverticulitis by ultrasound is made by identifying the following findings: colon wall thicker than 5mm, fat enhancement, evidence of abscess, visualized diverticuli, air artifacts suggesting diverticuli, and tenderness with compression of the probe.6 Diagnosis of diverticulitis by CT is made by identifying the following findings: colonic wall thickening, pericolic fat stranding, abscess formation and enhancement of the colonic wall. Often, these signs are associated with an identifiable inflamed diverticulum.7
Aortic Dissection Case Report
DOI: https://doi.org/10.21980/J8964ZIn transverse view, point-of-care ultrasound (POCUS) showed an anechoic circular true lumen (blue highlight) and half-circular anechoic false lumen (green highlight), separated by a near hyperechoic dissection flap (orange highlight) that pulsated with blood flow. When viewed in sagittal orientation, the anechoic true lumen (blue highlight) appears longitudinal, separated from the false lumen (green highlight) by a dissection flap (orange highlight). Stills showing the measurements of these dissections are also provided.
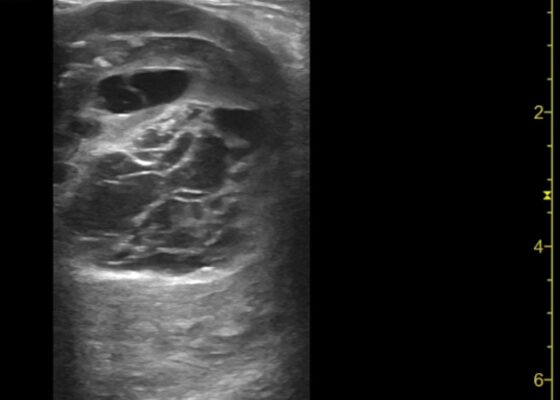
Thigh Mass Case Report
DOI: https://doi.org/10.21980/J8QD3CPoint-of-care ultrasound (POCUS) demonstrates a large, subcutaneous mass with areas of mixed echogenicity. The mass contains fluid-filled, anechoic areas with internal septations and absent doppler flow. The majority of the mass appears isoechoic to the surrounding tissues with a hyperechoic border. Computed tomography (CT) of his right thigh shows a 16 x 8.1 x 9.5 cm heterogenous, complex mass within his hamstring muscles, inferior to the femur. His lab work was significant for a white blood cell (WBC) of 17.3 (103/µL).
A Case Report of May-Thurner Syndrome Identified on Abdominal Ultrasound
DOI: https://doi.org/10.21980/J8C64KThe patient initially received a venous doppler ultrasound that showed no evidence of a right or left femoropopliteal venous thrombus. Due to the high suspicion of a DVT given the symmetric swelling to the entire limb and acute onset of pain, a CTV was ordered. The transverse view of the CTV showed chronic thrombotic occlusion of the proximal left common iliac vein associated with compression from the right common iliac artery (figure 1, transverse image of CTA), as well as thrombotic occlusion of the left internal iliac vein tributary and corresponding left ascending lumbar vein. Given the previously mentioned clinical context, these features suggested the diagnosis of May-Thurner syndrome.
Vitreous Hemorrhage Case Report
DOI: https://doi.org/10.21980/J88D3BPoint of care ultrasound (POCUS) revealed hyperechoic material in the vitreous consistent with a vitreous hemorrhage. On the ultrasound images, there is visible hyperechoic debris seen floating in the vitreous as the patient moves his eye. Since the vitreous is typically anechoic (black) in color on ultrasound, turning up the gain on the ultrasound machine makes these findings easier to see and often highlights abnormalities, such as this hemorrhage (see annotated still).