Neurology
Case Report of a Patient Presenting with Nonketotic Hyperglycemia Hemichorea
DOI: https://doi.org/10.21980/J8.52115Laboratory tests indicated elevated blood glucose levels (198 mg/dL) with no urinary ketones, anion gap of 12, thyroid stimulating hormone (TSH) of 12 UIU/ml, and an increased glycated hemoglobin (HbA1c) of 14.9%. After initial stroke evaluation with neurology, imaging studies, including computed tomography (CT)/CT angiography (CTA) of the brain and neck, were unremarkable, ruling out structural lesions or acute stroke. Neurology recommended an MRI which showed T1 shortening within the left basal ganglia involving both the caudate nucleus and the lentiform nucleus. T1 shortening indicates changes in the tissue composition or structure that alters how the tissue responds to the MRI pulse, giving the tissue a brighter appearance on MRI (see white arrow).
Beware of the Pediatric Limp: A Case of Mycoplasma Associated Acute Transverse Myelitis
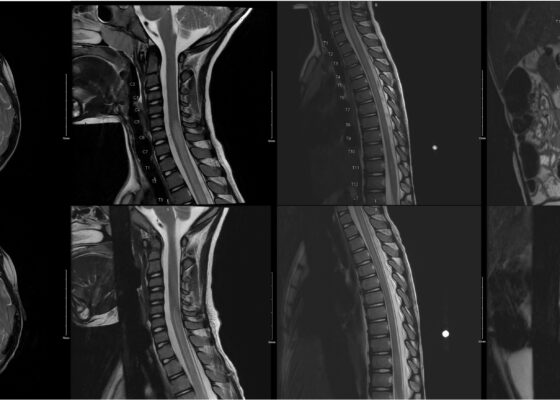
DOI: https://doi.org/10.21980/J8QQ1QAn MRI with contrast, T2 sequence was performed. In Figures a-d, the MRI of the patient’s brain and spinal cord on admission shows abnormal signals in the patient’s pons (lack of symmetrical gray-white differentiation on cross-section) along with hyperintensity (sagittally shown as brightness in what should be homogenously intense spinal cord) and significant central cord edema (with swelling seen as increased width) starting from C5 and continuing to the conus medullaris around L1/L2.
Eye-Opener: A Case Report of Eyelid Taping as Presenting Symptom of Myasthenia Gravis
DOI: https://doi.org/10.21980/J8NW8GPhysical exam was significant for a very pleasant, well-appearing female in no acute distress, noted to have clear plastic tape attached to her bilateral eyelids and brows (Image 1). When the tape was removed, she had bilateral ptosis, more significantly in the left eye (Image 2). She had no conjunctival injection or pallor. Her airway was patent and protected. She had no neck masses or carotid bruits. Her heart and lung exams were normal, with no evident respiratory distress. Her neurologic exam was further significant for limited extra-ocular movement (EOM). Her most notable deficits were with lateral and upward gaze (Video 1) indicative of weakness at the muscles innervated by cranial nerves III and VI. Her pupillary response was symmetric and brisk bilaterally. She had no additional cranial nerve deficits, slurred speech, or asymmetry in her strength or sensation throughout.
Subarachnoid Hemorrhage Causing a Seizure: An Assessment Simulation for Medical Students
DOI: https://doi.org/10.21980/J8XH1HAt the conclusion of the simulation leaners will be able to: 1) efficiently take a history from the patient and perform a physical exam (including a complete neurological exam); 2) identify red flag symptoms in a patient complaining of a headache; 3) order and interpret the results of a CT of the head and either a CT angiogram of the brain or a lumbar puncture to make the diagnosis of subarachnoid hemorrhage; 4) demonstrate appropriate management of a seizure; and 5) utilize the I-PASS framework to communicate with the inpatient team during the transition of care.
The Clue is in the Eyes. A Case Report of Internuclear Ophthalmoplegia
DOI: https://doi.org/10.21980/J8DP9MThere was no appreciable esotropia or exotropia noted on straight gaze (yellow arrows). On extraocular muscle examination, patient was noted to have a complete left medial rectus palsy consistent with a left internuclear ophthalmoplegia (red arrow). This was evidence by both eyes easily gazing left (green arrows); however, with rightward gaze, her left eye failed to gaze past midline (red arrow).