Issue 4:2
Point-of-Care Ultrasound for the Diagnosis of Systolic Heart Failure
DOI: https://doi.org/10.21980/J8HD1RBedside ultrasound with the phased array probe was used to obtain a parasternal long axis view which demonstrated poor contractility and a severely decreased ejection fraction (EF). M-mode was placed over the anterior leaflet of the mitral valve to create a tracing depicting both the E-wave of early diastole (green arrow) and the A-wave from the atrial kick (blue arrow). The shortest distance between the septum and the mitral valve on the M-mode tracing gives the patient’s E-Point Septal Separation (EPSS) (pink arrow). EF can be estimated using the formula EF=75.5-2.5 x EPSS (in mm). This patient’s EPSS was measured to be 20mm which estimates that she had an EF of 25.5%.
Bedside Ultrasound for the Rapid Diagnosis of Fournier’s Gangrene
DOI: https://doi.org/10.21980/J8CP99Point of care ultrasound (POCUS) utilizing a high-frequency linear probe revealed heterogeneous debris with subcutaneous air within the scrotal wall extending into the perineum consistent with necrotizing fasciitis of the perineum or Fournier’s gangrene (FG). The video shows multiple foci of gas that appear as echogenic dots with “dirty shadows” posteriorly from reverberation artifact arising from gas within the soft tissue.
Pneumocystis jirovecii (carinii) Pneumonia
DOI: https://doi.org/10.21980/J8RW6NChest X-ray showed diffuse, patchy interstitial and alveolar infiltrates bilaterally concerning for Pneumocystis jirovecii(previously Pneumocystis carinii) pneumonia (PJP). The AP radiograph (top left figure) showed the classic “bat-wing” distribution on the left side. Repeat radiograph (bottom figure) one day after admission showed worsening of the infiltrates.
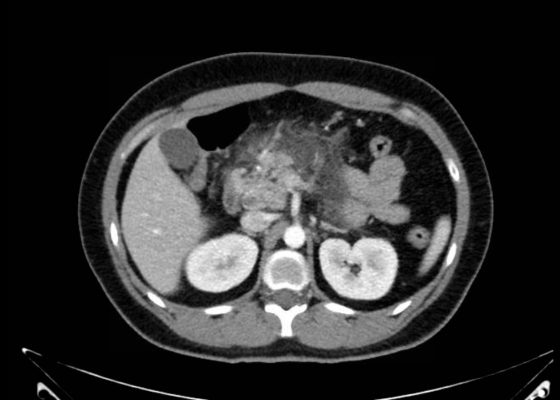
Acute Pancreatitis
DOI: https://doi.org/10.21980/J88W5XComputed tomography of the abdomen and pelvis with contrast show edema of the pancreas (red outline) and duodenum (yellow arrow) with peripancreatic inflammation, fluid and fat stranding (blue highlight). The distal pancreatic tail was noted to appear normal (green arrow). There was no organized drainable fluid collection, and no parenchymal hypo-enhancement. These findings are consistent with moderate severity acute interstitial pancreatitis.
Renal and Splenic Infarcts
DOI: https://doi.org/10.21980/J8804KOn the coronal sections of computed tomography (CT), bilateral renal infarctions (blue arrows) and several splenic infarctions (green arrows) are noted. Of particular interest, part of the clot totally occluding the left renal artery visibly extends into the aorta (red arrow). The vascular reconstruction image is remarkable for the absent left kidney, the unusual contour of the right kidney and the abnormal splenic blush.
Erectile Dysfunction as a Presenting Symptom for Renal Cell Carcinoma
DOI: https://doi.org/10.21980/J8563BThe MRI showed extensive spondylotic changes suggestive of malignancy (red arrows) with severe spinal canal stenosis at the lumbar spine L3-L4 (purple arrows) level contributing to clumping of cauda equina nerve roots and severe bilateral neuroforaminal narrowing with diffuse disc bulges abutting the exiting nerve roots at multiple levels. Findings also showed a hypo-attenuated tumor (blue arrow) and hyper-attenuated loculated tumor (green arrow) consistent with renal cell carcinoma (RCC).
Pectoralis Muscle Tendon Rupture
DOI: https://doi.org/10.21980/J81D01There is a noticeable difference in appearance and location of maximal prominence of the right pectoral muscle with arms outstretched (image 1). This is accentuated by having the patient perform an isometric arm press. (image 2).There is absence of the anterior axillary fold with adduction against resistance. The stump of the pectoralis muscle was palpated along his armpit. He otherwise has full range of motion in the shoulder with minimal pain.
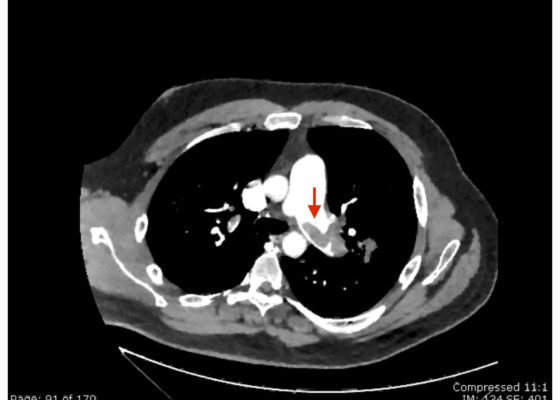
Saddle Pulmonary Embolus
DOI: https://doi.org/10.21980/J8N63PAn electrocardiogram (ECG) showed evidence of right heart strain with an incomplete right bundle branch block, S1Q3T3 (see red arrow [S1], blue arrow [Q3], and black arrow [T3]), and ST-segment elevation in the septal leads (green arrows). Bedside echocardiography showed a dilated right ventricle with ventricular wall akinesis (red arrow) sparing the apex (purple arrow), which is known as McConnell’s Sign. It also showed a mobile hyperechoic mass (yellow arrow). These ultrasound findings were concerning for pulmonary embolism (PE), so computed tomography (CT) angiogram of the chest was ordered and confirmed massive bilateral obstructive filling defects (red arrows) consistent with saddle pulmonary embolism. Additionally, noted is flattening of the interventricular septum (blue arrow) consistent with right heart strain. Laboratory studies were notable for a troponin-I of 0.29 ng/mL, a B-type natriuretic peptide of 792.3 pg/mL, lactic acid of 5.30 mmol/L, and a creatinine of 2.0 mg/dL, consistent with end organ dysfunction. All other lab work was within normal limits.