Infectious Disease
Fitz Hugh Curtis Case Report
DOI: https://doi.org/10.21980/J82K9GA sagittal view from computed tomography (CT) of the abdomen and pelvis demonstrated fat stranding beneath the inferior margin of the liver (outlined in red). The axial view showed fat stranding adjacent to the ascending colon without significant colon wall thickening (arrow). Fat stranding can occur as a hazy increased attenuation (brightness) or a more distinct reticular pattern.
Peritonsillar Abscess Model for Ultrasound Diagnosis Using Inexpensive Materials
DOI: https://doi.org/10.21980/J86G9PBy the end of this instructional session learners should be able to: 1) identify and discuss the indications, contraindications, and complications associated with peritonsillar abscesses, 2) properly identify and measure a PTA through ultrasound, and 3) competently perform ultrasound-guided peritonsillar abscess drainage on a simulator and remove fluid.
Spinal Epidural Abscess
DOI: https://doi.org/10.21980/J8T938After this simulation case, learners will be able to diagnose and manage patients with spinal epidural abscesses. Specifically, learners will be able to: 1) Obtain a detailed history, including past infectious, surgical, procedural and social history to evaluate for epidural abscess risk factors; 2) describe clinical signs and symptoms of spinal epidural abscesses and understand that initial clinical presentations can be variable;
3) perform a focused neurological exam including evaluation of motor, sensory, reflexes, and rectal tone; 4) order appropriate laboratory testing and imaging modalities for spinal epidural abscess diagnosis, including a post-void bladder residual volume; 5) select appropriate antibiotics for empiric treatment of spinal epidural abscess depending on patient presentation; 6) disposition the patient to appropriate inpatient care.
Case Report: Acute Supraglottitis
DOI: https://doi.org/10.21980/J8006VOn arrival, radiographs of the neck soft tissues were obtained, which showed a markedly enlarged epiglottic shadow (red arrow) concerning for epiglottitis. A computed tomography scan of the neck soft tissues with contrast was then obtained which revealed edematous mucosal thickening of the oropharynx (blue arrow) and supraglottic larynx (green arrow) including the epiglottis (purple arrow) concerning for acute infectious pharyngitis and supraglottic laryngitis with severe narrowing of the supraglottic laryngeal lumen, as well as associated extensive inflammation and edema of the superficial and deep left neck spaces. The patient’s white blood cell count was elevated to 25.7x109/L with 87% neutrophils. Her rapid strep test was positive. Otolaryngology was consulted and performed a bedside flexible laryngoscopy which showed significant edema of the epiglottis (orange arrow), vocal cords (white arrow), and arytenoids (black arrow), left greater than right. Based on the findings and concern for impending respiratory failure, the patient received an awake fiberoptic intubation by anesthesia at the bedside.
Emergency Medicine Curriculum Utilizing the Flipped Classroom Method: Infectious Disease and Immunology
DOI: https://doi.org/10.21980/J8DD1TWe aim to teach the presentation and management of infectious disease and immunological emergencies through the creation of a flipped classroom design. The topics include sepsis, sexually transmitted infections (STIs), tropical diseases, angioedema and anaphylaxis, transplant-related emergencies, and collagen vascular diseases. This unique, innovative curriculum utilizes resources chosen by education faculty and resident learners, study questions, real-life experiences, and small group discussions in place of traditional lectures. The goal of our curriculum is to encourage self-directed learning, improve understanding and knowledge retention, and improve the educational experience of our residents.
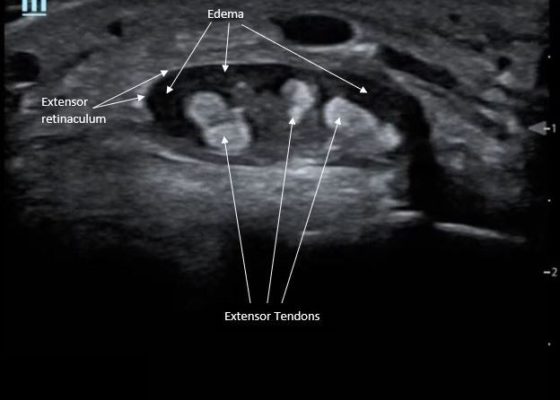
Point-Of-Care Ultrasound for the Diagnosis of Extensor Tenosynovitis
DOI: https://doi.org/10.21980/J8Q050Point-of-care ultrasound of the dorsal aspect of the left hand reveals a heterogenous hypoechoic fluid collection surrounding the extensor tendons (axial view) within the retinaculum consistent with edema. Longitudinal view shows anechoic fluid within the tenosynovium which is located between the anisotropic extensor tendon and linear hyperechoic synovial sheath. Longitudinal view also shows some cobblestoning, or tissue edema, superficial to the anisotropic extensor tendon. The patient’s contralateral right dorsal hand was scanned in a longitudinal view and shows no cobblestoning or hypoechoic fluid under the synovial sheath. The patient was diagnosed with tenosynovitis, and started on intravenous antibiotics.
Oral Herpes Zoster
DOI: https://doi.org/10.21980/J8QS69Physical exam findings revealed vesicular lesions on the lip, hard and soft palates which did not cross the midline. The lesions appeared in the distribution of the maxillary branch (V2) of the trigeminal nerve, consistent with herpes zoster.
Bedside Ultrasound for the Rapid Diagnosis of Fournier’s Gangrene
DOI: https://doi.org/10.21980/J8CP99Point of care ultrasound (POCUS) utilizing a high-frequency linear probe revealed heterogeneous debris with subcutaneous air within the scrotal wall extending into the perineum consistent with necrotizing fasciitis of the perineum or Fournier’s gangrene (FG). The video shows multiple foci of gas that appear as echogenic dots with “dirty shadows” posteriorly from reverberation artifact arising from gas within the soft tissue.