X-Ray
Loose PEG Tube Leading to Peristomal Leakage and Peritonitis
DOI: https://doi.org/10.21980/J8HS7TFrontal chest X-ray showed a large radiolucent area (pink highlighted area) underneath the diaphragm (yellow line) and on top of the liver (blue highlighted area) and spleen (green highlighted area) suggestive of pneumoperitoneum possibly caused by gastrointestinal perforation. This large radiolucent area can also be seen underneath the diaphragm in the lateral view chest X-ray. Computed tomography (CT) was not performed due to his physical exam findings and the significant positive findings on chest X-ray. Surgery was consulted and patient was taken emergently to the operating room.
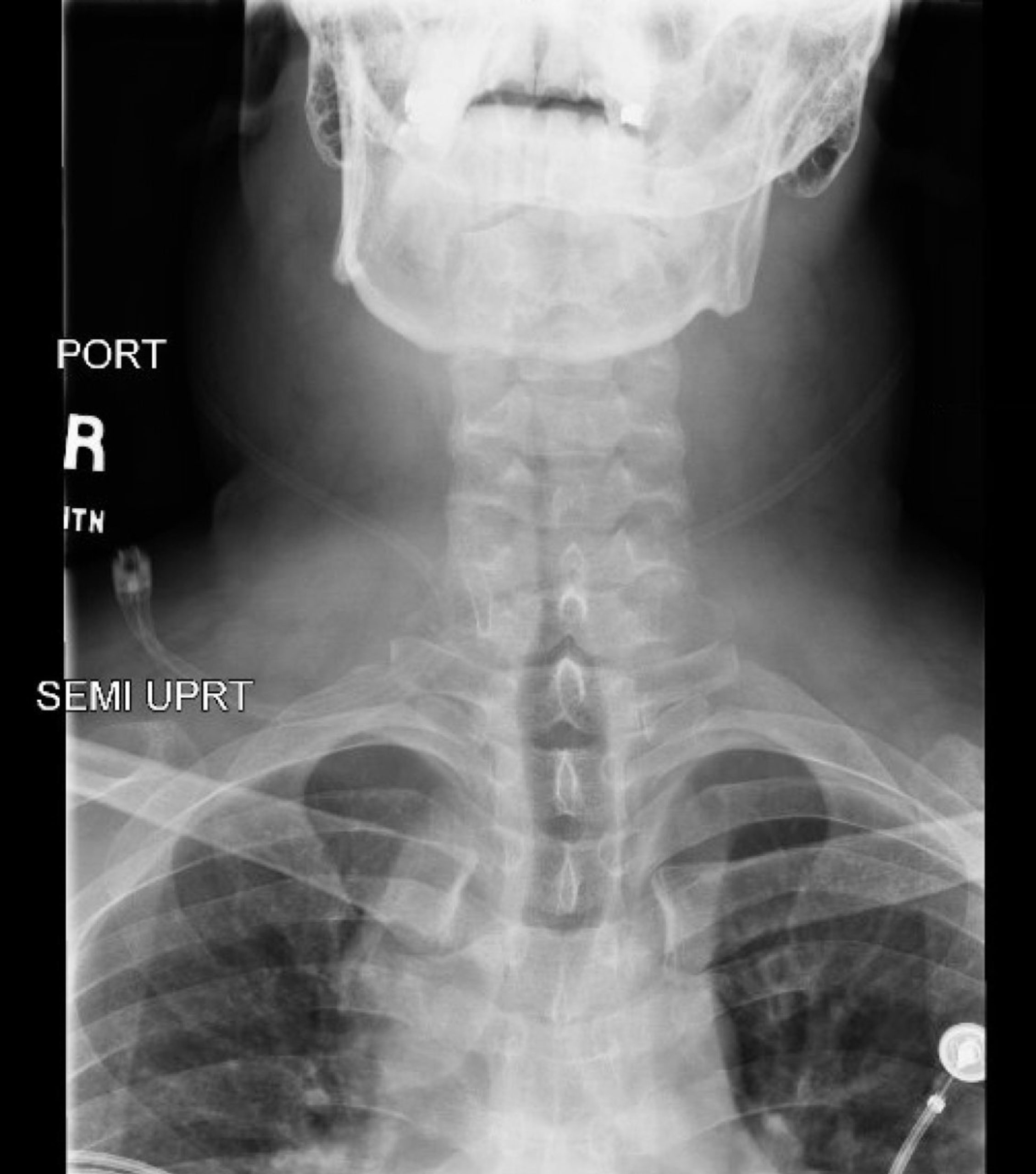
Rapid Airway Narrowing Associated with Hodgkin’s Lymphoma
DOI: https://doi.org/10.21980/J86D3QNeck X-ray showed nonspecific significant prevertebral soft tissue swelling at the level of the cervical spine, with associated apparent thickening of the epiglottis (yellow arrow), diffuse soft tissue swelling of the neck (red arrows) and tracheal airway narrowing (light blue arrow). The computed tomography imaging of the neck was significant for multiple conglomerating pathological lymph nodes with a significant mass effect (orange arrows) compressing the right internal jugular vein (green arrow).
Ascending Thoracic Aortic Dissection: A Case Report of Rapid Detection Via Emergency Echocardiography with Suprasternal Notch Views
DOI: https://doi.org/10.21980/J8WW6WVideo of parasternal long-axis bedside transthoracic echocardiogram: The initial images showed grossly normal left ventricular function, and no pericardial effusion or evidence of cardiac tamponade. However, the proximal aorta beyond the aortic valve was poorly-visualized in this window.
Case Report: Acute Supraglottitis
DOI: https://doi.org/10.21980/J8006VOn arrival, radiographs of the neck soft tissues were obtained, which showed a markedly enlarged epiglottic shadow (red arrow) concerning for epiglottitis. A computed tomography scan of the neck soft tissues with contrast was then obtained which revealed edematous mucosal thickening of the oropharynx (blue arrow) and supraglottic larynx (green arrow) including the epiglottis (purple arrow) concerning for acute infectious pharyngitis and supraglottic laryngitis with severe narrowing of the supraglottic laryngeal lumen, as well as associated extensive inflammation and edema of the superficial and deep left neck spaces. The patient’s white blood cell count was elevated to 25.7x109/L with 87% neutrophils. Her rapid strep test was positive. Otolaryngology was consulted and performed a bedside flexible laryngoscopy which showed significant edema of the epiglottis (orange arrow), vocal cords (white arrow), and arytenoids (black arrow), left greater than right. Based on the findings and concern for impending respiratory failure, the patient received an awake fiberoptic intubation by anesthesia at the bedside.
Digital Nerve Block for the Reduction of a Proximal Phalanx Fracture of the Foot – a Case Report
DOI: https://doi.org/10.21980/J8KS8TPlain film of the right foot showed evidence of an oblique fracture of the body of the proximal 4th phalanx (image 2). No other acute traumatic injuries noted in the rest of the bones and joints of the right foot. After performing a digital block of the toe and reduction, repeat imaging showed evidence of successful reduction with anatomic alignment and redemonstration of the fracture line (image 3).
Open Subtalar Dislocation
DOI: https://doi.org/10.21980/J87P8PX-ray of the left ankle revealed a complete dislocation of the subtalar joint with medial dislocation of the calcaneus (outlined in orange) relative to the talus (outlined in red) with subcutaneous air noted in the lateral soft tissues (blue arrows in Figure 1). The talonavicular joint has also been disrupted (navicular outlined in blue). There was no evidence of fracture. Post-reduction computed tomography of the left lower extremity confirmed no evidence of associated fracture.
Medial Subtalar Dislocation: A Case Report
DOI: https://doi.org/10.21980/J8QP9DOn examination, the patient had a significant deformity to his left foot and ankle. His left foot was pointed medially. His distal left tibia and fibula were visible and palpable upon inspection, with the overlying skin completely intact. There was no neurovascular compromise of the foot. X-ray demonstrated a subtalar dislocation of the left ankle (green arrow) and significant widening of the tibiotalar joint space (yellow arrow). There was associated soft tissue swelling but no acute displaced fractures were identified.
Traumatic Diaphragmatic Rupture – A Case Report
DOI: https://doi.org/10.21980/J8G64HChest X-ray showed an elevated left hemi-diaphragm with superior displacement of a portion of intra-abdominal contents presumed to be the stomach (green arrowheads) with associated rightward mediastinal shift (yellow arrows). The diagnosis was confirmed by CT. Computed tomography imaging of the chest showed a large, left diaphragmatic defect measuring approximately 5.5 cm with herniation of the upper half of the stomach through the defect. The fundus of the stomach (blue arrow) herniated superiorly through the ruptured diaphragm (red arrow).