Ultrasound
A Case Report of Neonatal Vomiting due to Adrenal Hemorrhage, Abscess and Pseudohypoaldosteronism
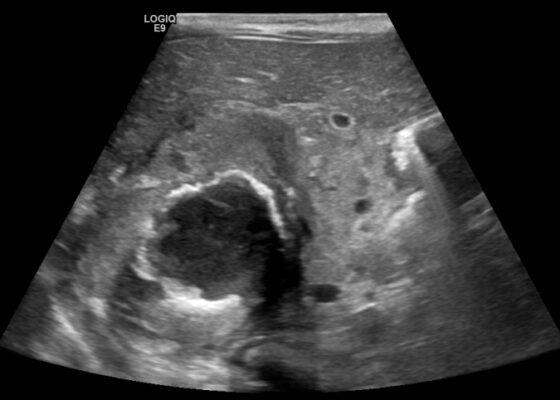
DOI: https://doi.org/10.21980/J8QQ0BAn ultrasound (US) of the abdomen was obtained to evaluate for possible pyloric stenosis (see US transverse/dopper imaging). While imaging showed a normal pyloric channel, it revealed an unexpected finding: a complex cystic mass arising from the right adrenal gland (yellow outline), measuring 5.8 by 4.0 by 6.4 cm with calcifications peripherally and mass effect on the kidney without evidence of vascular flow (blue arrow). Computed tomography (CT) of the abdomen/pelvis with IV contrast was subsequently obtained and measured the lesion as 2.8 by 4.6 by 4 cm without evidence of additional masses, lymphadenopathy or left adrenal gland abnormality (see CT axial, coronal, and sagittal imaging).
Case Report of Unusual Facial Swelling in an 8-Month-Old
DOI: https://doi.org/10.21980/J8M06FFacial ultrasound revealed local inflammatory changes such as increased echogenicity and heterogeneity in the soft tissues of the right cheek, suggestive of soft tissue edema. There was evidence of a prominent right parotid gland with increased heterogeneity suggestive of a traumatic injury. Additionally, facial ultrasound demonstrated a 6mm ill-defined anechoic collection within the right cheek without increased doppler flow (green arrow), thought to represent a focal area of edema instead of an abscess.
Point of Care Ultrasound as a Diagnostic Tool to Detect Small Bowel Obstruction in the Emergency Department: A Case Report
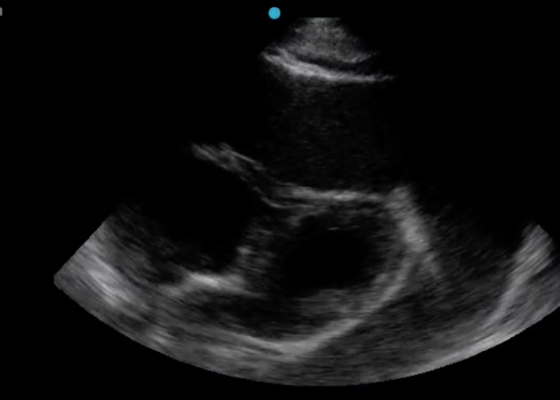
DOI: https://doi.org/10.21980/J8XD1GThe ultrasound findings suggestive of small bowel obstruction (SBO) are typically visualized in video; however, certain still images can also demonstrate SBO including greater than three dilated loops of small bowel (>2.5 cm), thickened-walled bowel (>3 mm), visualization of plicae circulares, and extraluminal fluid caused by inflammatory changes along the bowel wall, which are all highly suggestive of SBO.3
In this patient’s case, we were able to visualize several dilated loops of small bowel (red arrow) with oscillating intraluminal contents known as “Whirl Sign.” Additionally, we were able to visualize extraluminal fluid, demonstrated as an anechoic triangular-shaped collection. The characteristic shape of this triangular shaped collection of fluid is known as a “Tanga Sign,” given its name due to way it looks similar to the lower half of a bikini (blue arrow). Tanga sign can occur when the loops of dilated bowel appear prominent in contrast to the inflammatory extraluminal fluid in an SBO. These ultrasound findings were highly concerning for SBO which was later confirmed on CT imaging of the abdomen, which demonstrated SBO with a transition point in the left lower quadrant.
A Case Report of Cardiac Tamponade
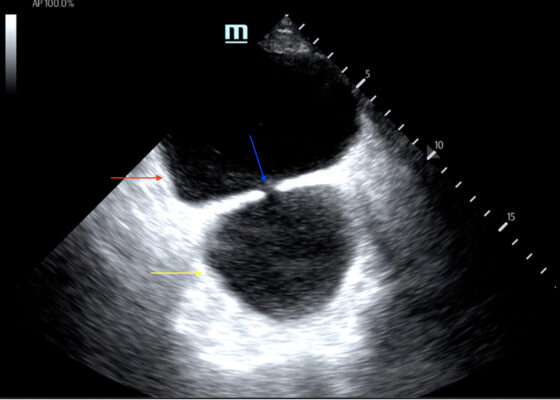
DOI: https://doi.org/10.21980/J8J644The patient was in noticeable respiratory distress and had oxygen saturation of 94% on room air. Bilateral jugular venous distention with severe right supraclavicular lymphadenopathy and diffuse bilateral wheezing was present. Although muffled heart sounds and hypotension are part of Beck’s Triad, these were not present in this case. Electrocardiogram obtained on arrival showed a sinus tachycardia with low-voltage QRS complexes and electrical alternans. Low voltage QRS can be seen on the ECG provided and is demonstrated by the low amplitude of the QRS complexes seen on all the leads. Electrical alternans may have an alternating axis or amplitudes of the QRS complex. Alternating axis is best visualized in V4-V6 on this ECG while alternating amplitudes are seen throughout the rest of the ECG. Computed tomography angiogram (CTA) of the chest revealed a large pericardial effusion with bilateral pulmonary emboli and a right upper lobe mass. A bedside transthoracic echocardiogram (TTE) was then performed and confirmed the large effusion, but also showed right ventricular collapse during diastole, indicative of cardiac tamponade.
Using Point-of-Care Ultrasound to Expedite Diagnosis of Necrotizing Fasciitis: A Case Report
DOI: https://doi.org/10.21980/J85051A consultative scrotal ultrasound was performed, which was read as showing a small right hydrocele, small bilateral scrotal pearls, and normal-appearing testes. Although present, there was no mention of subcutaneous air suggestive of NF, seen in figure 1 as punctate hyperechoic foci (arrowhead) with ring-down artifact known as dirty shadowing (arrow). Also, subcutaneous thickening (asterisk) and free fluid (arrow) were seen as shown in figure 2, although their clinical relevance was not recognized in the radiologist's final report. Figure 3 shows an abdominal and pelvic CT that re-demonstrates subcutaneous air in the scrotum and lower abdomen (arrow) as well as fascial thickening of the perineum and free intra-abdominal air. After these images, the patient was transferred to our hospital for further management. Almost immediately after the patient's arrival, POCUS was employed. As seen in figures 4, we were able to identify in just a few minutes extensive subcutaneous air accompanied by dirty shadowing, as well as re-demonstration of subcutaneous thickening, fluid collections, and a right hydrocele. Even without the outside hospital's CT, the sonographic findings were highly suggestive for the diagnosis of NF of the perineum, also known as Fournier’s gangrene.
A Case Report on Detecting Porcelain Gallbladder form Wall-Echo-Shadow Sign on Point-of-Care Ultrasound
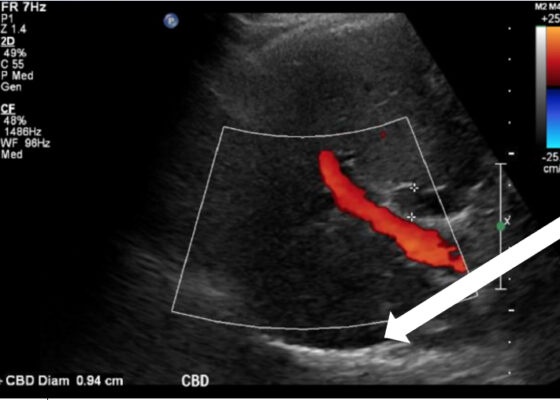
DOI: https://doi.org/10.21980/J8164GPoint-of-care ultrasound (POCUS) was performed by the emergency physician. Gallbladder ultrasound (US) should be performed using a curvilinear probe. If the patient’s body habitus does not allow for the use of a curvilinear probe, a phased array probe may be used. To find the gallbladder with ultrasonography, two approaches are commonly used. Many physicians prefer the “subcostal sweep” in which the probe is placed on the xiphoid process in a sagittal plane and swept along the inferior costal margin until the gallbladder is visualized. If this does not adequately locate the gallbladder, the “X minus 7” approach may be used. In this approach, the probe is placed on the xiphoid (X) process in a transverse view and moved 7 centimeters (minus 7) to the patient’s right. This technique is useful for patients with a larger body habitus. If the gallbladder is still not visualized, placing the patient in left lateral decubitus position or asking them to take a deep breath and hold may help the ultrasonographer locate the gallbladder. The US revealed mild hepatic biliary duct dilation with cholelithiasis and sludge, but no additional evidence to suggest cholecystitis. The US image showed a dilated common bile duct at 0.94 cm and calcifications. Visualization of the gallbladder wall is essential in differentiating between a positive wall-echo-shadow (WES) sign and a porcelain gallbladder. While a hypoechoic gallbladder wall is indicative of a WES sign, a hyperechoic wall layer will indicate a calcified gallbladder wall, suggesting a porcelain gallbladder. In image 1, the hyperechoic gallbladder wall can be visualized (white arrow), suggesting the presence of porcelain gallbladder and distinguishing it from a positive WES sign.
Bladder Diverticulum – A Case Report
DOI: https://doi.org/10.21980/J8635COn examination, the patient was alert and oriented but in mild distress. Suprapubic fullness was noted upon abdominal palpation. Point of care ultrasound of the bladder showed two enlarged “bladders” with a central communication. Bedside total bladder volume was measured to be 1288 cm3 (the top “bladder” was measured to be 1011 cm3, while the bottom “diverticulum” was measured to be 277 cm3) by ultrasound.
The POCUS stills of the patient’s bladder demonstrated the bladder (red arrow) and bladder diverticulum (yellow arrow) with a central communication (blue arrow) in the transverse and sagittal views.
Ascending Thoracic Aortic Dissection: A Case Report of Rapid Detection Via Emergency Echocardiography with Suprasternal Notch Views
DOI: https://doi.org/10.21980/J8WW6WVideo of parasternal long-axis bedside transthoracic echocardiogram: The initial images showed grossly normal left ventricular function, and no pericardial effusion or evidence of cardiac tamponade. However, the proximal aorta beyond the aortic valve was poorly-visualized in this window.