Thoracic Aortic Aneurysm Measured by Point of Care Ultrasound Suprasternal Notch View
History of present illness:
A 39-year-old male presented to the emergency department (ED) with chest pressure, diaphoresis, and dizziness. He was found to be hypertensive with a blood pressure of 210/105 in the primary care office and was sent to the emergency department, where on arrival his blood pressure was 175/108. He was found to have a non-ischemic EKG, and he reported a family history significant for aortic aneurysms to the provider. Patient was obese but had no other pertinent physical exam findings.
Significant findings:
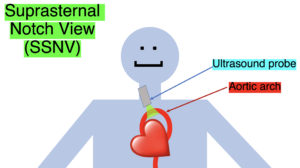
Point-of-care cardiac echocardiogram demonstrated a dilated ascending aorta (illustrated in red) measuring approximately 4 cm in the parasternal long axis (PLAX). A dilated aortic arch (illustrated in green) also measuring approximately 4 cm was appreciated using the suprasternal notch view (SSNV). A follow-up computed tomography angiogram (CTA) was performed, validating bedside ultrasound measurements.
Discussion:
Aortic aneurysms are prevalent in about 5% of the population, with risk factors including age, atherosclerosis, and concomitant thrombotic disease processes such as coronary artery disease and peripheral vascular disease. Lifestyle risk factors such as smoking have also been identified as associated with aortic aneurysms.1
The diagnostic criteria for dilated thoracic aneurysm is based on multiple factors including age, sex, and body size.2 An aortic root diameter of ³ 4.0 cm constitutes an ascending aortic dilation.3,4 Point-of-care cardiac and SSNV ultrasound of the thoracic aorta has been validated as an accurate study when performed by emergency physicians to identify thoracic aortic aneurysms (sensitivity of 71.4%, specificity of 100% when compared to gold standard of CTA). 5 This case is an example of the utility of rapid bedside diagnostic ultrasound, specifically the SSNV, in assessment of thoracic aneurysms.
The current guidelines recommend medical versus surgical management of a thoracic aortic aneurysm based on stability. Medical management is recommended in patients who are asymptomatic with ascending aorta greater than 5.5cm in diameter. This is achieved by managing hypertension with beta blockers to maintain blood pressure less than 140/90 mmHg, and managing dyslipidemia with statins. Surgical management is generally recommended in patients with ascending aortic aneurysms greater than 5.5cm in diameter or in those with unstable dilation measuring greater than 0.5 cm/year. 6
Point-of-care cardiac echocardiography demonstrated a dilated ascending aorta. Finding a new thoracic aortic aneurysm in the setting of chest pain and hypertension is a “can’t miss” diagnosis due to the potential for rapid expansion leading to dissection and/or rupture.6 Point-of-care ultrasound utilizing the SSNV is a tool that can be used early in the evaluation of the patient that can help make quick determination of diagnostic plan and expedite initiating treatment in the emergency department.
This patient was treated with bolus injections of labetalol 10mg in the ED which achieved a goal blood pressure of 140s/80s mmHg and resolved his chest pressure. The patient was admitted and transitioned to labetalol 100mg by mouth three times daily, which adequately controlled his blood pressure. Repeat imaging showed no change in the size of the aneurysm over the subsequent 24 hours, and he was ultimately discharged with medical management and follow up.
Topics:
Ultrasound, thoracic aneurysm, suprasternal notch view.
References:
- Lindholt JS, Sørensen J, Søgaard R, Henneberg EW. Long-term benefit and cost-effectiveness analysis of screening for abdominal aortic aneurysms from a randomized controlled trial. Br J Surg. 2010;97(6):826-834.
- Hannuksela M, Lundqvist S, Carlberg B. Thoracic aorta–dilated or not? Scand Cardiovasc J. 2006;40(3):175-178. doi: 10.1080/14017430600565999.
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(41):2873-2926. doi: 10.1093/eurheartj/ehu281.
- Labovitz AJ, Noble VE, Bierig M, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23(12):1225-1230. doi: 10.1016/j.echo.2010.10.005.
- Kinnaman KA, Kimberly HH, Pivetta E, et al. Evaluation of the aortic arch from the suprasternal notch view using focused cardiac ultrasound. J Emerg Med. 2016;50(4):643-650.e1. doi: 10.1016/j.jemermed.2015.12.002.
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010;121(13): E43-86. doi: 10.1161/CIR.0b013e3181d4739e.