Visual EM
Septic Arthritis of the Acromioclavicular Joint: A Case Report
DOI: https://doi.org/10.21980/J8VP9NMagnetic resonance imaging (MRI) with contrast was obtained of the shoulder and ankle, and results from both scans showed findings consistent with septic arthritis complicated by intraarticular abscesses. The MRI of the patient’s left acromioclavicular joint is shown as both a T1-weighted sequence in sagittal view and T2-weighted sequence in coronal view. The images show effusion (the dark fluid denoted by the red arrow) with an adjacent fluid collection (blue arrow). A T2-weighted MRI in coronal view of the patient’s right ankle showing multiple effusions (green arrows) and a fluid collection along the medial tibial cortex and subcutaneous tissues (yellow arrow).
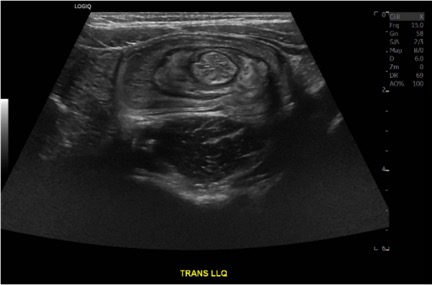
Case Report of a Child with Colocolic Intussusception with a Primary Lead Point
DOI: https://doi.org/10.21980/J8564QOn the initial ED visit, an abdominal ultrasound (US) was ordered which showed the classic intussusception finding of a target sign (yellow arrow), or concentric rings of telescoped bowel, on the transverse view of the left lower quadrant (LLQ).
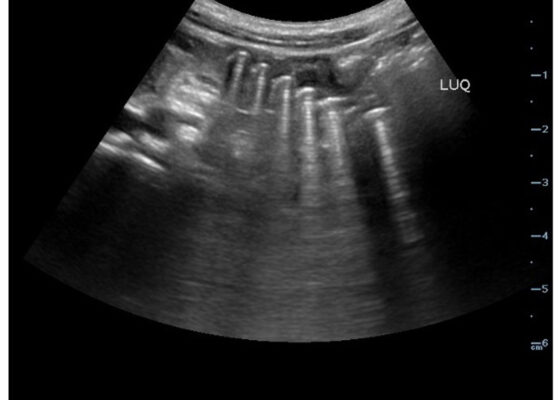
Point-Of-Care Ultrasound Use for Detection of Multiple Metallic Foreign Body Ingestion in the Pediatric Emergency Department: A Case Report
DOI: https://doi.org/10.21980/J83D2DBedside POCUS was performed on the patient’s abdomen using the curvilinear probe. The left upper quadrant POCUS image demonstrates multiple hyperechoic spherical objects with shadowing and reverberation artifacts concerning multiple foreign body ingestions. Though the patient and mother initially denied knowledge of foreign body ingestion, on repeated questioning after POCUS findings, the patient admitted to his mother that he ate the spherical magnets he received for his birthday about one week ago. The patient swallowed these over the course of two days. The presence of multiple radiopaque foreign bodies was confirmed with an abdominal X-ray.
Sonographic Retrobulbar Spot Sign in Diagnosis of Central Retinal Artery Occlusion: A Case Report
DOI: https://doi.org/10.21980/J8735PThe bedside ocular ultrasound (B-scan) was significant for small, hyperechoic signal (white arrow) in the distal aspect of the optic nerve, concerning for embolus in the central retinal artery. Subsequent direct fundoscopic exam was significant for a pale macula with cherry red spot (black arrow), consistent with central retinal artery occlusion (CRAO).
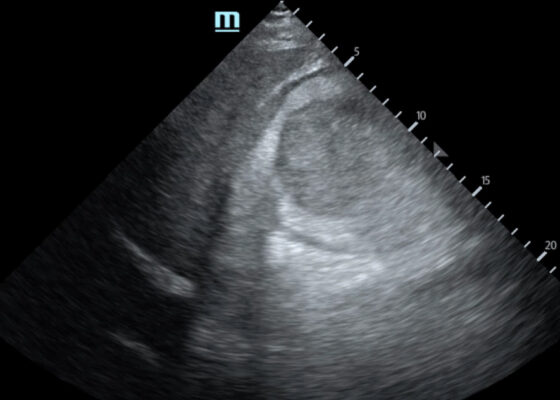
Trauma by Couch: A Case Report of a Massive Traumatic Retroperitoneal Hematoma
DOI: https://doi.org/10.21980/J84D2QUpon arrival at the trauma center, a FAST revealed a large, well-circumscribed abnormality (red outline) deep to the liver (blue outline and star) and gallbladder (green outline and star). The right kidney and hepatorenal space were not clearly visualized. The remainder of the FAST showed no free fluid in the splenorenal space, pelvis, and no pericardial effusion. He had lung sliding bilaterally.
A Case Report of Invasive Mucormycosis in a COVID-19 Positive and Newly-Diagnosed Diabetic Patient
DOI: https://doi.org/10.21980/J81M1GOn physical exam, when the patient was asked to try and look to her right, the right eye failed to move laterally/abduct (blue arrow). Additionally, when asked to look straight ahead, the eye was slightly adducted (red arrow). There was a lack of motion of the right eye in abduction when the patient was asked to look to her right (yellow arrow).
A Patient with Generalized Weakness – A Case Report
DOI: https://doi.org/10.21980/J8593CThe CT of the abdomen and pelvis showed evidence of a large subcapsular rim-enhancing fluid collection with multiple gas and air-fluid levels along the right kidney measuring 8 x 4 cm axially and 11 cm craniocaudally (blue outline) with mass effect on the right renal parenchyma (yellow outline). Another suspected fluid collection adjacent to the upper pole of the right kidney measuring 4 x 3.4 cm was noted (red outline). Bilateral pyelonephritis was suggested without hydronephrosis or nephrolithiasis. The findings suggested complicated pyelonephritis with emphysematous abscess and hematoma formation.
A Case Report of Subtle EKG Abnormalities in Acute Coronary Syndromes Indicative of Type One Myocardial Infarction
DOI: https://doi.org/10.21980/J8W06XThe ECG does show multiple subtle abnormalities that in conjunction with his symptoms and risk factors are concerning for ischemia and/or occlusion of the coronary artery vessel. 1) ST depression in aVL. Although slight, the ST segment is below the TP segment or isoelectric point (blue circles). 2) Focal hyper QT waves. The T-waves in II, III, AVF V2, V3, and V4 are hyper acute, namely peaked and tall in relationship to the QRS. These are best displayed in leads II, III, and AVF where the T-waves are taller than the QRS amplitude (vertical blue lines). 3) Straightening off the ST segment. Multiple leads display a straight ST segment namely aVL, III, AVF, and V2 (red lines). Of note, the length of the straight ST segment is greater than 1/4 the amplitude of the QRS (purple lines). 4) Although subtle, these abnormalities are focal in nature.