Cardiology/Vascular
ECG Stampede
DOI: https://doi.org/10.21980/J8PP93ECG Stampede is a unique educational program comprised of a comprehensive, video-based curriculum with accompanying student and instructor guides. ECG Stampede also features an engaging game accessible via modern browsers and dedicated mobile applications for iOS and Android devices. The gamified model presents learners with a batch of ECGs for which they must assign one of four triage acuities.
Atypical Presentation of Abdominal Aortic Aneurysm
DOI: https://doi.org/10.21980/J82W6FBedside ultrasound revealed an abdominal aortic aneurysm (AAA) with concern for dissection vs thrombus/hematoma due to an area of echogenicity within the lumen of the vessel, since normal blood vessels (including the aorta) have lumens that are uniformly anechoic. An intimal flap concerning for dissection appears as a hyperechoic stripe within the lumen of the vessel on ultrasound, often with a hypoechoic and/or anechoic area appreciated underneath the flap, indicating a separate area of blood flow. If this visualized area is of significant size, color doppler can be used to confirm blood flow on both sides of the flap. Given his bedside ultrasound findings, the patient underwent emergent computed tomography scan and was found to have an enlarged infrarenal abdominal aortic aneurysm, with acute intramural hematoma, extending into bilateral common iliac arteries.
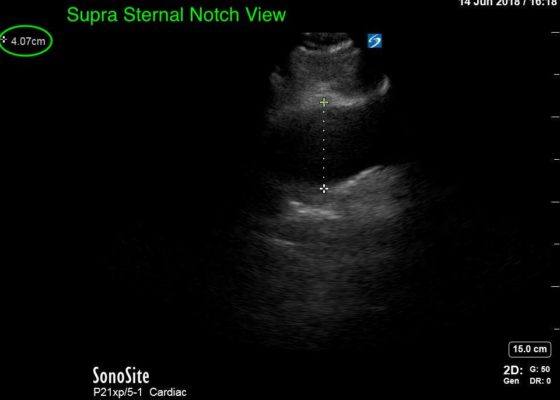
Thoracic Aortic Aneurysm Measured by Point of Care Ultrasound Suprasternal Notch View
DOI: https://doi.org/10.21980/J8Z64VPoint-of-care cardiac echocardiogram demonstrated a dilated ascending aorta (illustrated in red) measuring approximately 4 cm in the parasternal long axis (PLAX). A dilated aortic arch (illustrated in green) also measuring approximately 4 cm was appreciated using the suprasternal notch view (SSNV). A follow-up computed tomography angiogram (CTA) was performed, validating bedside ultrasound measurements.
A Story About Mesenteric Ischemia
DOI: https://doi.org/10.21980/J8J33QWe aim to teach the presentation and management of cardiovascular emergencies through the creation of a flipped classroom design. This unique, innovative curriculum utilizes resources chosen by education faculty and resident learners, study questions, real-life experiences, and small group discussions in place of traditional lectures. In doing so, a goal of the curriculum is to encourage self-directed learning, improve understanding and knowledge retention, and improve the educational experience of our residents.
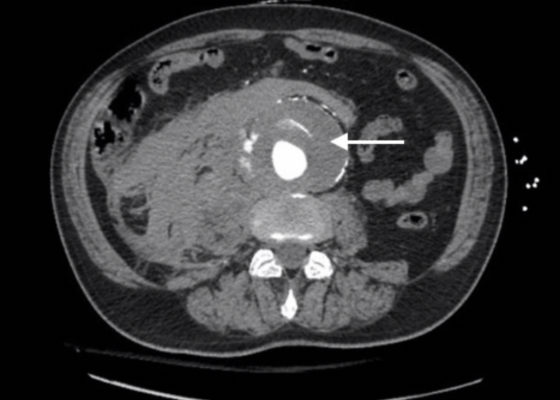
Ruptured AAA Presenting with Unresponsiveness and Cardiac Arrest
DOI: https://doi.org/10.21980/J8M34QAxial CT images from the CT chest, abdomen and pelvis revealed a large infra-renal abdominal aortic aneurysm measuring 7.3 x 8.2 x 10 cm with extensive mural thrombus (single white arrow) that has ruptured, with active extravasation (black arrow) of contrast into the aneurysm sac and retroperitoneum with large right retroperitoneal hematoma (multiple white arrows).
Levamisole Induced, Cocaine Associated Vasculitis
DOI: https://doi.org/10.21980/J8K35SAn asymmetric pattern of palpable purpura with bullae was noted on bilateral lower extremities with smaller patches on bilateral upper extremities. There was no tenderness or crepitus.
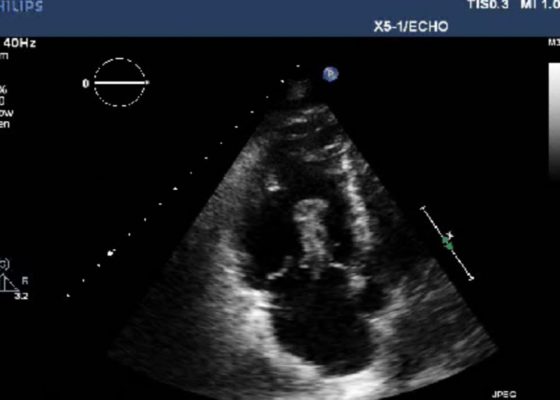
Right Atrial Thrombus
DOI: https://doi.org/10.21980/J8F93V History of present illness: A 77-year-old male presented to the emergency department with shortness of breath. Symptoms progressively worsened over the last 4-5 days, and on arrival was associated with chest tightness. He denied any medical conditions, smoking, or pertinent family history. He has not seen a primary care physician in “many years.” Upon arrival he was in mild
Point-of-Care Ultrasound for the Diagnosis of Systolic Heart Failure
DOI: https://doi.org/10.21980/J8HD1RBedside ultrasound with the phased array probe was used to obtain a parasternal long axis view which demonstrated poor contractility and a severely decreased ejection fraction (EF). M-mode was placed over the anterior leaflet of the mitral valve to create a tracing depicting both the E-wave of early diastole (green arrow) and the A-wave from the atrial kick (blue arrow). The shortest distance between the septum and the mitral valve on the M-mode tracing gives the patient’s E-Point Septal Separation (EPSS) (pink arrow). EF can be estimated using the formula EF=75.5-2.5 x EPSS (in mm). This patient’s EPSS was measured to be 20mm which estimates that she had an EF of 25.5%.