Tricuspid Annular Plane Systolic Excursion (TAPSE) in a Patient with Pulmonary Emboli
History of present illness:
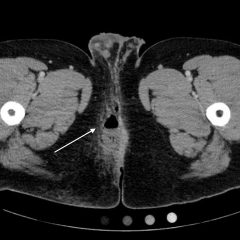
A 60-year-old male with a history of pulmonary emboli (PE) presented to the emergency department with exertional shortness of breath following a ten-hour flight. The patient admitted to recently stopping his previously prescribed rivaroxaban. His electrocardiogram (ECG) showed findings consistent with a S1Q3T3 pattern. Point-of-care ultrasound (POCUS) was performed using the curvilinear probe, which revealed a thrombus in the inferior vena cava (IVC). POCUS using the phased array probe demonstrated an abnormal tricuspid annular plane systolic excursion (TAPSE) and a significantly dilated right ventricle (RV). Computed tomography angiogram (CTA) showed evidence of acute emboli within the right and left distal main pulmonary arteries, left lobar, and left proximal segmental artery. Additionally, a thrombus was visualized in the left distal subhepatic IVC. The patient was admitted to telemetry for anticoagulation and monitoring. Right heart catheterization revealed a significantly elevated pulmonary artery pressure of 95/27.
Significant findings:
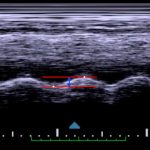
Video 1 and Image 1 show a thrombus in the patient’s IVC. Video 2 and Images 2-3 demonstrate a positive TAPSE of less than 17mm (blue arrow length) with a significantly dilated RV, indicating abnormal excursion of the tricuspid annulus and right ventricular dysfunction.
Discussion:
Pulmonary embolism is the third leading cause of death from cardiovascular disease following myocardial infarction and stroke.1 Approximately half of all PEs are diagnosed in the emergency department2 and early detection and treatment have been shown to improve outcomes and survival.3 Pulmonary emboli can present with a wide range of symptoms including dyspnea, chest pain, shock, or sustained hypotension, and can even be asymptomatic, making it a potentially challenging diagnosis.4 Studies show a high specificity of over 80% but low sensitivity of lower than 60%, for echocardiography in the diagnosis of PE, making it a potentially useful rule-in test that can be done at the bedside prior to CT.5 Echocardiography looks for various signs of right heart strain which could be indicative of a PE. However, it cannot be used to rule out the diagnosis of PE, since a method with a higher sensitivity is needed.
Although not commonly used in the bedside diagnosis of PE, TAPSE has been found to have a sensitivity of up to 94% in detecting right heart strain in patients with tachycardia or hypotension.6 To measure TAPSE, one must obtain an apical four-chamber view of the heart and use M mode to measure the longitudinal displacement of the lateral tricuspid annulus during systole and diastole. M mode will generate a sine wave that can be measured from peak to trough. Measurements less than 17mm are considered positive, suggestive of right heart systolic dysfunction and are associated with a poor prognosis in patients with PE, particularly in those with tachycardia or hypotension.
Depending on the size and location of the embolus, the clinical presentation of PE can range from asymptomatic to right ventricular failure, cardiogenic shock, and death. The embolus causes hypoxia and the release of vasoactive mediators which cause localized vasoconstriction. This produces an increase in afterload for the right ventricle, which can lead to right ventricular failure and subsequent hypotension and shock.7 In these hemodynamically unstable patients, thrombolytic therapy should be considered for more rapid improvements in right ventricular function and pulmonary perfusion.8 Utilizing a quick and sensitive modality such as TAPSE can aid in making these time sensitive decisions in the management of PE.
Topics:
Pulmonary embolism, ultrasound, TAPSE, POCUS, right ventricular dysfunction, right heart strain, IVC, thrombus.
References:
- Goldhaber S, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379(9828):1835-1846. doi: 10.1016/S0140-6736(11)61904-1
- Pollack CV, Schreiber D, Goldhaber SZ, Slattery D, Fanikos J, O’Neil BJ, et al. Clinical characteristics, management, and outcomes of patients diagnosed with acute pulmonary embolism in the emergency department: initial report of EMPEROR (Multicenter Emergency Medicine Pulmonary Embolism in the Real World Registry). Appl Clin Inform. 2011;57(6)700-6. doi: 10.1016/j.jacc.2010.05.071
- Roy PM, Meyer G, Vielle B, Le Gall C, Verschuren F, Carpentier F, et al. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med. 2006;144(3)157-164. doi: 10.7326/0003-4819-144-3-200602070-00003
- Agnelli G, Becattini C. Acute pulmonary embolism. N Engl J Med. 2010;363(3):266-274. doi: 10.1056/NEJMra0907731
- Fields JM, Davis J, Girson L, Au A, Potts J, Morgan CJ, et al. Transthoracic echocardiography for diagnosing pulmonary embolism: a systematic review and meta-analysis. J Am Soc Echocardiogr. 2017;30(7):714-723. doi: 10.1016/j.echo.2017.03.004
- Daley J, Grotberg J, Pare J, Medoro A, Liu R, Hall MK, et al. Emergency physician performed tricuspid annular plane systolic excursion in the evaluation of suspected pulmonary embolism. Am J Emerg Med. 2017;35(1):106-111. doi: 10.1016/j.ajem.2016.10.018
- Matthews JC, McLaughlin V. Acute right ventricular failure in the setting of acute pulmonary embolism or chronic pulmonary hypertension: a detailed review of the pathophysiology, diagnosis, and management. Curr Cardiol Rev. 2008;4(1):49-59. doi: 10.2174/157340308783565384
- Fesmire FM, Brown MD, Espinosa JA, Shih RD, Silvers SM, Wolf SJ, et al. Critical issues in the evaluation and management of adult patients presenting to the emergency department With suspected pulmonary embolism. Ann Emerg Med. 2011;57(6):628-652. doi: 10.1016/j.annemergmed.2011.01.020