Abdominal/Gastroenterology
Gastric Volvulus
DOI: https://doi.org/10.21980/J8335FPoint of care ultrasound of his abdomen showed a large fluid filled structure with well-defined borders containing gastric contents extending from the xiphoid process to the umbilical region. No free fluid was noted on focus assessment with sonography for trauma (FAST) examination. A computed tomography (CT) scan was performed emergently and it was noted that the patient had a significantly distended stomach and gastric volvulus (blue arrows) noted in the area of his paraesophageal/hiatal hernia.
Wandering Spleen
DOI: https://doi.org/10.21980/J8PS7CHistory of present illness: A 7-month-old boy presented for evaluation of an abdominal mass. Two weeks prior, the patient had a fever followed by 24 hours of vomiting and abdominal pain, which self-resolved. His pediatrician noted the mass on exam and referred child to the emergency department (ED). His abdominal exam was significant for a hard mass palpated to the
Acute Pancreatitis
DOI: https://doi.org/10.21980/J88W5XComputed tomography of the abdomen and pelvis with contrast show edema of the pancreas (red outline) and duodenum (yellow arrow) with peripancreatic inflammation, fluid and fat stranding (blue highlight). The distal pancreatic tail was noted to appear normal (green arrow). There was no organized drainable fluid collection, and no parenchymal hypo-enhancement. These findings are consistent with moderate severity acute interstitial pancreatitis.
Renal and Splenic Infarcts
DOI: https://doi.org/10.21980/J8804KOn the coronal sections of computed tomography (CT), bilateral renal infarctions (blue arrows) and several splenic infarctions (green arrows) are noted. Of particular interest, part of the clot totally occluding the left renal artery visibly extends into the aorta (red arrow). The vascular reconstruction image is remarkable for the absent left kidney, the unusual contour of the right kidney and the abnormal splenic blush.
Sigmoid Diverticulitis Complicated by Colovesical Fistula Presenting with Pneumaturia
DOI: https://doi.org/10.21980/J80G9TA CT scan of his abdomen/pelvis shows acute sigmoid colonic diverticulitis with adjacent extraluminal collection containing gas (axial view, white arrow) consistent with perforation, along with abutment of the urinary bladder with intraluminal bladder gas (sagittal and coronal views, white arrowheads) suggesting colovesical fistula.
Brief Review of Intussusception Diagnosis and Management
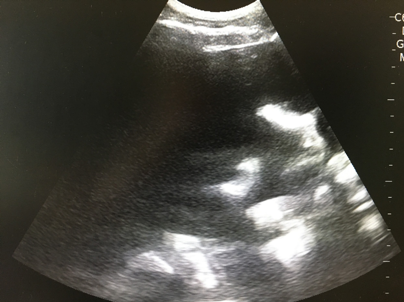
DOI: https://doi.org/10.21980/J81P7FThe patient’s abdominal ultrasound revealed intussusception in the right upper abdominal quadrant. The transverse ultrasound view showed a “doughnut sign” (dashed yellow line), telescoping bowel (yellow arrow), and invaginated hyperechoic mesenteric fat with crescent configuration (dashed orange line). The sagittal ultrasound view demonstrated the intussusception formed by the outer recipient bowel loop (yellow arrows), invaginated hyperechoic mesenteric fat (orange asterisks), and telescoping bowel centrally (red arrow).
Realistic and Inexpensive Ultrasound Guided Paracentesis Simulator Using Pork Belly with Skin
DOI: https://doi.org/10.21980/J8NK9RBy the end of this instructional session learners should be able to: 1) Discuss the indications, contraindications, and complications associated with abdominal paracentesis; and 2) competently perform an ultrasound-guided abdominal paracentesis on a simulator and remove fluid.
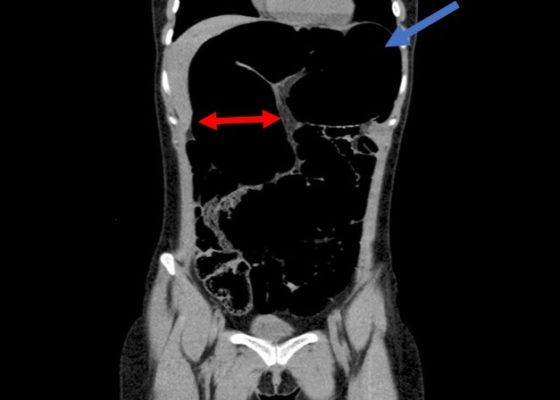
Recurrent Sigmoid Volvulus in a Young Female
DOI: https://doi.org/10.21980/J8GW5SComputed tomography (CT) of the abdomen and pelvis was obtained revealing a colonic volvulus in the left mid to upper abdomen (blue arrow) involving the distal transverse colon and descending colon, with gaseous colonic distention to 8.5 cm (red arrow). The characteristic “whirl pattern” is also present (yellow arrow). These findings are suggestive of a high-grade colonic obstruction. It was without evidence of pneumoperitoneum, pneumatosis, or drainable collection. Of note, a 3.6 cm dermoid tumor is also observable in the left adnexa (green arrow).