Issue 8:1
Telemedicine Consult for Shortness of Breath Due to Sympathetic Crashing Acute Pulmonary Edema
DOI: https://doi.org/10.21980/J8HS86At the completion of the simulation and debriefing, the learner will be able to: 1) recognize the physical exam findings and presentation of SCAPE, 2) utilize imaging and laboratory results to further aid in the diagnosis of SCAPE, 3) initiate treatments necessary for the stabilization of SCAPE, 4) demonstrate the ability to assist with the stabilization and disposition of a patient via tele-medicine as determined by the critical action checklist and assessment tool below, 5) interpret the electrocardiogram (EKG) as atrial fibrillation with rapid ventricular response (AFRVR), and 6) recognize that SCAPE is the underlying cause of AFRVR and continue to treat the former.
Anticholinergic Toxicity in the Emergency Department
DOI: https://doi.org/10.21980/J8D07ZBy the end of this simulation case, learners will be able to: 1) describe the classic clinical presentation of anticholinergic toxicity, 2) discuss common medications and substances that may lead to anticholinergic toxicity, 3) recognize the electrocardiogram (ECG) findings in anticholinergic toxicity that require specific therapy, and 4) review the management of anticholinergic toxicity.
The Suicidal Patient in the Emergency Department Team-Based Learning Activity
DOI: https://doi.org/10.21980/J8892XBy the end of the session, participants will be able to: 1) describe risk factors for suicide; 2) summarize the emergency physician’s role in assessing patients with psychiatric emergencies; 3) assess a patient using a mental status evaluation; 4) identify the criteria for involuntary psychiatric hold placement; 5) develop a safe discharge plan for patients experiencing depression; and 6) Formulate a plan for evaluating a suicidal patient who is acutely intoxicated.
Child Maltreatment Education: Utilizing an Escape Room Activity to Engage Learners on a Sensitive Topic
DOI: https://doi.org/10.21980/J84H1CBy the end of the escape room, the learner should be able to: 1) understand the national and local prevalence of child maltreatment; 2) understand the different types of child maltreatment and common associated presentations; 3) know the local EMS agency reporting requirements; 4) understand when to make base hospital contact with respect to concern for maltreatment; 5) collaborate effectively as a team.
Acute Chest Syndrome
DOI: https://doi.org/10.21980/J80S8JAt the end of this oral board session, examinees will: 1) demonstrate the ability to obtain a complete medical history; 2) demonstrate the ability to perform a detailed physical examination in a patient with respiratory distress; 3) identify a patient with respiratory distress and hypoxia and manage appropriately (administer oxygen, place patient on monitor); 4) investigate the broad differential diagnoses which include acute chest syndrome, pneumonia, acute coronary syndrome, acute congestive heart failure, acute aortic dissection and acute pulmonary embolism; 5) list the appropriate laboratory and imaging studies to differentiate acute chest syndrome from other diagnoses (complete blood count, comprehensive metabolic panel, brain natriuretic peptide (BNP), lactic acid, procalcitonin, EKG, troponin level, d-dimer, chest radiograph); 6) identify a patient with acute chest syndrome and manage appropriately (administer intravenous pain medications, administer antibiotics after obtaining blood cultures, emergent consultation with hematology) and 7) provide appropriate disposition to the intensive care unit after consultation with hematology.
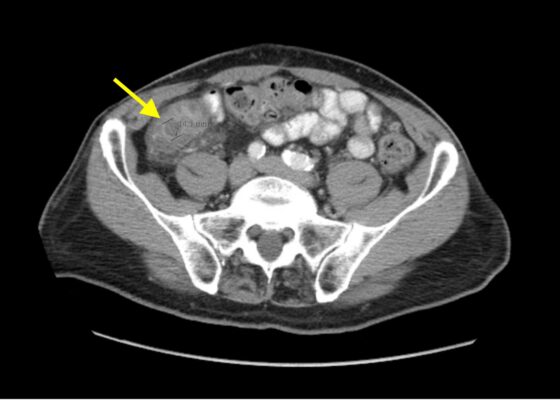
Imaging Findings of Small Bowel – Diverticulitis: A Case Report
DOI: https://doi.org/10.21980/J8F078Bedside ultrasound was performed and showed thickened bowel wall (orange marker), fat enhancement (green marker), and phlegmonous structure with central echogenicity (yellow marker). Imaging of the abdomen and pelvis with CT showed marked wall thickening and inflammatory change involving a 7.0cm segment of the distal/terminal ileum suspicious for severe ileitis with phlegmon and microabscess on the coronal image (yellow arrow). Additonally, the transverse images show a small rim-enhancing focus within this region of inflammation measuring up to 1.4cm which could represent microabscess (yellow arrow). Diagnosis of diverticulitis by ultrasound is made by identifying the following findings: colon wall thicker than 5mm, fat enhancement, evidence of abscess, visualized diverticuli, air artifacts suggesting diverticuli, and tenderness with compression of the probe.6 Diagnosis of diverticulitis by CT is made by identifying the following findings: colonic wall thickening, pericolic fat stranding, abscess formation and enhancement of the colonic wall. Often, these signs are associated with an identifiable inflamed diverticulum.7
Aortic Dissection Case Report
DOI: https://doi.org/10.21980/J8964ZIn transverse view, point-of-care ultrasound (POCUS) showed an anechoic circular true lumen (blue highlight) and half-circular anechoic false lumen (green highlight), separated by a near hyperechoic dissection flap (orange highlight) that pulsated with blood flow. When viewed in sagittal orientation, the anechoic true lumen (blue highlight) appears longitudinal, separated from the false lumen (green highlight) by a dissection flap (orange highlight). Stills showing the measurements of these dissections are also provided.
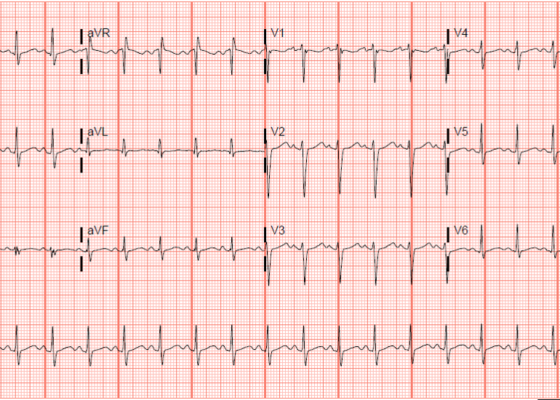
Electrocardiogram Abnormalities Following Diphenhydramine Ingestion: A Case Report
DOI: https://doi.org/10.21980/J85H1PThe blue arrow points to one of the terminal R waves in aVR, and the green arrow points to one of the large S waves in lead I, indicating right axis deviation. These findings are pathognomonic for sodium channel blockade. Due to the specific ECG findings and knowledge of diphenhydramine overdose, it was evident that these ECG findings were due to a cardiac sodium channel blockade. Sodium channels are essential within myocardial tissue to ensure the rapid upstroke of cardiac action potential, as well as rapid impulse conduction throughout cardiac tissue. Therefore, sodium channel blockers tend to exhibit significant dysrhythmic properties due to severe conduction disturbances.2 The blockage of the cardiac sodium channels appears as terminal R waves in aVR as well as terminal S waves in lead I due to delaying, and possibly blocking, the electrical conduction pathway of the heart. The orange arrows show resolution of terminal R wave in aVR and terminal S wave in lead I, after administration of sodium bicarbonate.
Epilepsy Caused by Neurocysticercosis: A Case Report
DOI: https://doi.org/10.21980/J81P96In our patient, two lesions were most notable on CT in the frontal and occipital lobes. The lesion in the left frontal lobe (blue circle) was an approximately 1.5 centimeter (cm) rounded area with rim enhancement and surrounding hypodensity, consistent with vasogenic edema. A similar sized low-density area in the left occipital lobe (red circle) was noted, with increased peripheral density at the 3 o’clock position representing calcification. There were no areas of apparent hemorrhage or midline shift. The final radiology report concluded there were multiple cystic lesions, one with surrounding vasogenic edema in the left frontal lobe.
A Case of Community-Acquired Tuberculosis in an Infant Presenting with Pneumonia Refractory to Antibiotic Therapy
DOI: https://doi.org/10.21980/J8X07MChest radiographs during the initial presentation at seven weeks of life demonstrated right lower lobe (RLL) air space opacity on both PA and lateral views, compatible with pneumonia (referenced by yellow and green arrows, respectively). Repeat chest radiograph performed 12 days after the initial imaging revealed persistent right lower lobe opacity and right hilar fullness, seen as an opacified projection off of the mediastinal border as compared with the prior image, concerning for lymphadenopathy (designated by the aqua arrow). On the third presentation, computed tomography (CT) of the chest with intravenous contrast found persistent right lower lobe consolidation, innumerable 2-3 mm nodules, and surrounding ground glass opacities. This is best visualized as scattered areas of hyperdensity in the lung parenchyma. Axial images confirmed the presence of right hilar as well as subcarinal lymphadenopathy (indicated by white and pink arrows, respectively). Magnetic resonance imaging (MRI) of the brain with IV contrast was performed which showed a punctate focus of enhancement in the left precentral sulcus compatible with a tuberculoma (denoted with red arrow).
1›
Page 1 of 2