Achalasia: An Uncommon Presentation with Classic Imaging
History of present illness:
A 32-year-old male smoker with a BMI of 38.1 kg/m2, history of esophageal stricture, gastroesophageal reflux disease (GERD), and years of intermittent dry cough presented with three weeks of exacerbated, persistent cough worse in the morning and after eating. He denied fever, constitutional symptoms, dysphagia, or vomiting. He presented to the emergency department following an abnormal outpatient chest X-ray. Bilateral expiratory wheezing was noted on exam.
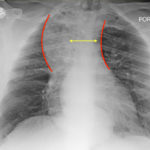
Significant findings:
The chest X-ray demonstrated a markedly widened mediastinum (red brackets), raising concern for thoracic aortic aneurysm/aortic dissection, which prompted labs and contrast-enhanced computed tomography (CT) of the chest. The CT revealed a dilated proximal esophagus that narrowed distally (yellow tracing and red arrow), with particulate material, mass-effect on the trachea (purple outline), and bilateral patchy opacities suggesting aspiration. Barium esophagram showed a drastically dilated esophagus filled with contrast (yellow arrow), terminating into the classic “bird’s beak sign” (red arrow) at the lower esophageal sphincter (LES). Esophageal manometry later confirmed achalasia, proving that widened mediastina can have unexpected etiologies.
Discussion:
Achalasia is a rare (prevalence ~0.3-9.5/100,000, increasing with age) digestive disorder characterized by denervation to the distal esophagus, promoting regional aperistalsis and tonic contraction of the LES.1-3 Achalasia most commonly presents as acute, simultaneous dysphagia to both solids and liquids, but can present as heartburn, regurgitation, or even unexplained cough.1-3 A dilated esophagus with narrowing at the LES (“Bird’s Beak Sign”) and delayed esophageal emptying on barium esophagram are pathognomonic for achalasia (sensitivity 90%, specificity 95%),4 as is distal aperistalsis with increased resting LES tone on high-resolution manometry (sensitivity 98%, specificity 96%).5 Pharmacologic LES relaxation may be trialed, but surgical myotomy is usually necessary.1,2,3,6 Our patient underwent laparoscopic Heller myotomy resulting in a dilated, aperistaltic esophagus with no evidence of obstruction and is being followed for continued GERD and dysphagia.
Topics:
Achalasia, widened mediastinum, acute dysphagia, barium esophagram, lower esophageal sphincter, esophageal dysmotility, aspiration, gastroenterology.
References:
- Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. 2014;383(9911):83-93. doi: 10.1016/S0140-6736(13)60651-0.
- Pandolfino JE and Gawron AJ. Achalasia – A Systematic Review. JAMA. 2015;313(18):1841–1852. doi:10.1001/jama.2015.2996.
- O’Neill OM. Achalasia: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2013;19(35):5806. doi:10.3748/wjg.v19.i35.5806.
- Gupta P, Debi U, Sinha SK, Prasad KK. Primary versus secondary achalasia: New signs on barium esophagogram. Indian J Radiol Imaging. 2015;25(3):288-295. doi:10.4103/0971-3026.161465.
- Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: A quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293(4): G878-G885. doi:10.1152/ajpgi.00252.2007.
- Arora Z, Thota PN, Sanaka MR. Achalasia: current therapeutic options. Therapeutic Advances in Chronic Disease. 2017;8(6-7):101-108. doi:10.1177/2040622317710010.