Bilateral Tibia/Fibula Fractures in Automobile versus Pedestrian Accident
History of present illness:
A 25-year-old female presented to the emergency department (ED) with bilateral lower extremity deformities after being struck by a car while riding a skateboard. The patient was not wearing a helmet but did not report a loss of consciousness. She endorses using methamphetamine and crack cocaine on the day of the accident. Examination of the right lower extremity revealed a 10cm x 7cm soft tissue injury with a 5cm segment of exposed tibia on the anteromedial aspect and a deep abrasion on the lateral aspect of the leg just superior to the patella. Examination of the left leg revealed a small 0.5cm x 0.5cm open wound on the anteromedial aspect of the tibia with oozing blood containing fat droplets and superficial abrasions over the knee. Dorsalis pedis and posterior tibial pulses were 2+ bilaterally. There was low suspicion of compartment syndrome, and there was no neurological deficit noted in the lower extremities.
Significant findings:
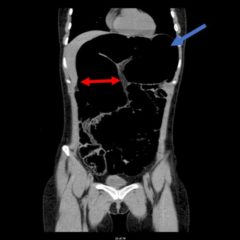
Plain film shows severely comminuted and displaced mid tibia/fibula fractures of bilateral lower extremities (red arrows) and comminuted right fibular head (blue arrow) and proximal shaft fracture (yellow arrow).
Discussion:
Limb trauma is one of the most common injuries seen in emergency medicine and is the most common reason for hospitalization in nonfatal traumas. Approximately 25% of tibial fractures are open, making the tibia the most common long-bone in which an open fracture occurs.1 The largest threat of limb loss is vascular injury. Bleeding can be controlled with direct pressure,2 a tourniquet,3,4 or clamping of the vessel. One should not attempt to clamp a vessel if it cannot be visualized.
If there are no signs of vascular injury requiring immediate surgery, nerves, bones, and soft tissues should be assessed. Sensation and strength should be evaluated to assess the integrity of the femoral, sciatic, deep fibular, and tibial nerves. Skin should be evaluated for lacerations, avulsions, penetrating injury, contamination, and open fractures.5 If there is extensive muscle damage, one must also monitor for signs of rhabdomyolysis.6
Extremity radiography is indicated if there is presence of deformity. Assessment should include the joint above and below the site of injury. Comminuted fractures increase the risk of arterial damage and such an injury should lead to a full vascular assessment.5 If the fracture is open, prophylactic antibiotic treatment should be started as the patient is at risk for osteomyelitis.7 Surgery is required for comminuted or open fractures. With casting only, comminuted fractures have an increased risk of nonunion, malunion, or shortening of the limb.8 Furthermore, by stabilizing the fracture, the soft tissues are stabilized, decreasing bacterial spread and inflammatory responses. Debridement of an open fracture is necessary to remove debris and unhealthy tissue from the wound.9
The patient in this case was given intravenous cefazolin and was taken to the operating room the same day by orthopedic surgery for bilateral lower extremity tibia and fibula open reduction and internal fixation.
Topics:
Tibia/fibula fracture, pedestrian vs. automobile, trauma.
References:
- Court-Brown CM, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg Br. 1995; 77:417-421.
- Bulger EM, Snyder D, Schoelles K, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014; 18:163-173. doi: 10.3109/10903127.2014.896962.
- Dorlac WC, DeBakey ME, Holcomb JB, et al. Mortality from isolated civilian penetrating extremity injury. J Trauma. 2005; 59:217-222. doi: 10.1097/01.TA.0000173699.71652.BA.
- Swan KG Jr, Wright DS, Barbagiovanni SS, Swan BC, Swan KG. Tourniquets revisited. J Trauma. 2009;66:672-675. doi: 10.1097/TA.0b013e3181986959.
- Schlickewei W, Kuner EH, Mullaji AB, Götze B. Upper and lower limb fractures with concomitant arterial injury. J Bone Joint Surg Br. 1992; 74:181-188.
- Keltz E, Khan F, Mann G. Rhabdomyolysis. The role of diagnostic and prognostic factors. Muscles Ligaments Tendons J. 2013;3(4):303-312.