CT
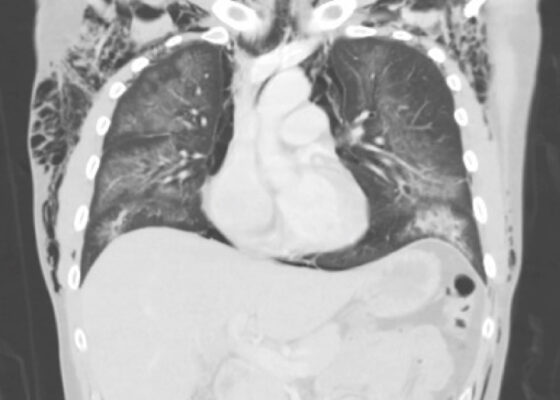
Electronic Cigarette or Vaping-Associated Lung Injury Case Report
DOI: https://doi.org/10.21980/J8S65PThe CT of the chest with contrast showed subcutaneous emphysema (green star), pneumomediastinum (yellow arrow), and pneumopericardium (purple asterix) without an identifiable tracheal tear. Extensive air was visualized as hypodense areas within the chest wall within the soft tissue. The image also detailed a hypodense area surrounding the heart consistent with pneumopericardium. No disruption of the trachea was present. Additionally, the CT of the chest also showed bilateral ground glass airspace opacities (red stars) with subpleural sparing that is consistent with EVALI findings.2,5 These specific findings have been seen in many of the EVALI cases.5 This image is interesting because there is extensive pneumomediastinum with no clearly identifiable cause. The imaging shows no esophageal or tracheal or lung injury, so it is important to note relevant information collected during interview regarding patient’s recent history of vaping THC, especially when establishing a differential diagnosis.
A Case Report of a Man with Burning Arm and Leg Weakness
DOI: https://doi.org/10.21980/J8V659A non-contrast computed tomography (CT) of the head and neck was performed, followed by an MRI of the cervical spine. The CT demonstrated congenital narrowing of the cervical spinal canal, with posterior disc osteophyte complex and disc bulge at C3-4 and C4-5 (arrow). The T2-weighted MRI additionally demonstrated obliteration of the anterior and posterior subarachnoid space at the level of C3-C5, with associated patchy central cord signal abnormality (arrow).
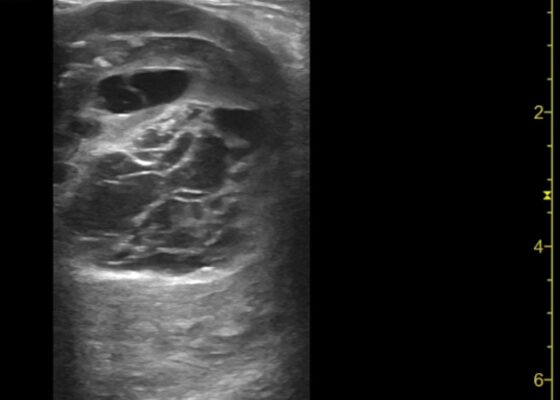
Thigh Mass Case Report
DOI: https://doi.org/10.21980/J8QD3CPoint-of-care ultrasound (POCUS) demonstrates a large, subcutaneous mass with areas of mixed echogenicity. The mass contains fluid-filled, anechoic areas with internal septations and absent doppler flow. The majority of the mass appears isoechoic to the surrounding tissues with a hyperechoic border. Computed tomography (CT) of his right thigh shows a 16 x 8.1 x 9.5 cm heterogenous, complex mass within his hamstring muscles, inferior to the femur. His lab work was significant for a white blood cell (WBC) of 17.3 (103/µL).
A Case Report of May-Thurner Syndrome Identified on Abdominal Ultrasound
DOI: https://doi.org/10.21980/J8C64KThe patient initially received a venous doppler ultrasound that showed no evidence of a right or left femoropopliteal venous thrombus. Due to the high suspicion of a DVT given the symmetric swelling to the entire limb and acute onset of pain, a CTV was ordered. The transverse view of the CTV showed chronic thrombotic occlusion of the proximal left common iliac vein associated with compression from the right common iliac artery (figure 1, transverse image of CTA), as well as thrombotic occlusion of the left internal iliac vein tributary and corresponding left ascending lumbar vein. Given the previously mentioned clinical context, these features suggested the diagnosis of May-Thurner syndrome.
A Case Report of Fournier’s Gangrene
DOI: https://doi.org/10.21980/J8Z356Physical exam revealed a comfortable-appearing male patient with tachycardia and a regular cardiac rhythm. The genitourinary exam indicated significant erythema and fluctuance of the bilateral lower buttocks with extension to the perineum. Black eschar and ecchymosis were also noted at the perineum. There was significant tenderness to palpation that extended beyond the borders of erythema. There was no palpable crepitus on initial examination. Physical exam was otherwise unremarkable.
Unravelling the Mystery of a Continuous Coil: A Case Report
DOI: https://doi.org/10.21980/J8PM00A CT scan of the abdomen and pelvis with intravenous contrast for evaluation of new onset abdominal pain and distension was obtained in the emergency department. The axial view (CT Image A) shows the coil pack from the prior coil-assisted retrograde transvenous obliteration procedure, seen in the left renal vein and gastric varix (red arrow). The path of the coil (yellow arrow) is continuous into the inferior vena cava (CT Image B). It is then seen (CT Image C) situated in the right ventricle (green arrow). Finally, the coil pack is seen in a coronal section, demonstrating its upward path (blue arrow) in the inferior vena cava. (CT Image D). Additional findings included ascites with advanced cirrhosis. As noted in the CT images, a vascular embolization coil was seen within a varix near the junction of the left renal vein. This appeared to have unraveled and extended superiorly into the inferior vena cava and ultimately into the right atrium and right ventricle.
Case Report of a Pelvic Kidney with Ureteral Obstruction from Inguinal Hernia Entrapment and Concurrent Cryptorchid Testis
DOI: https://doi.org/10.21980/J8F345The patient was afebrile with normal lactate and white blood cell count. Initial CT imaging showed an ectopic right pelvic kidney with entrapment of his right ureter within an indirect right inguinal hernia causing severe hydronephrosis (coronal: white arrow). Also discovered was an ovoid hypodensity in the right anterior pelvis consistent with right undescended testis (axial: orange arrow; coronal: green arrow) that was previously unknown to the patient, with a normal left scrotal testis (axial: red arrowhead; coronal: blue arrowhead). Other potential etiologies of the patient’s symptoms could include appendicitis or incarcerated inguinal hernia, though the imaging results and absence of systemic inflammatory response syndrome made these causes less likely.
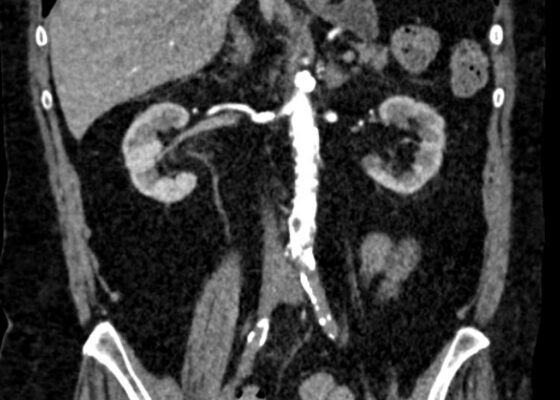
Initial Management and Recognition of Aortoiliac Occlusive Disease, A Case Report
DOI: https://doi.org/10.21980/J87M0ZComputerized tomography with angiography (CTA) of the entire aorta demonstrated an occluded distal infrarenal aorta with extension into the bilateral common femoral arteries (red outline), lack of flow through femoral arteries (yellow outline) and trickle flow reconstituted distally consistent with aortoiliac occlusive disease (blue outline). Some small segments of the proximal celiac axis showed signs of occlusion (purple outline). A short segment of non-specific bowel wall thickening, which may have been related to ischemic changes, was also seen (not seen on images). The included coronal slice shows the extent of the bilateral occlusive burden, with three-dimensional reconstruction emphasizing the same findings.