Respiratory
Modified Manikin for Tracheoinnominate Artery Fistula
DOI: https://doi.org/10.21980/J8Z93HBy the end of this educational session, learners will be able to: 1) perform a focused history and physical exam on any patient who presents with bleeding from the tracheostomy site; 2) describe the differential diagnosis of bleeding from a tracheostomy site, including a TIAF; 3) demonstrate the stepwise management of bleeding from a suspected TIAF, including cuff hyperinflation and the Utley Maneuver; 4) verify that definitive airway control via endotracheal intubation is only feasible in the tracheostomy patient when it is clear, upon history and exam, that the patient can be intubated from above; and 5) demonstrate additional critical actions in the management of a patient with a TIAF, including early consultation with otolaryngology and cardiothoracic surgery as well as emergent blood transfusion and activation of a massive transfusion protocol.
Tracheoinnominate Artery Fistula
DOI: https://doi.org/10.21980/J8K05RBy the end of this simulation, learners will be able to: 1) perform a focused history and physical exam on any patient who presents with bleeding from the tracheostomy site, 2) describe the differential diagnosis of bleeding from a tracheostomy site, including a TIAF, 3) demonstrate the stepwise management of bleeding from a suspected TIAF, including cuff hyperinflation and the Utley Maneuver, 4) verify that definitive airway control via endotracheal intubation is only feasible in the tracheostomy patient when it is clear, upon history and exam, that the patient can be intubated from above, 5) demonstrate additional critical actions in the management of a patient with a TIAF, including early consultation with otolaryngology and cardiothoracic surgery as well as emergent blood transfusion and activation of a massive transfusion protocol.
A Pediatric Emergency Medicine Refresher Course for Generalist Healthcare Providers in Belize: Respiratory Emergencies
DOI: https://doi.org/10.21980/J84063This curriculum presents a refresher course in recognizing and stabilizing pediatric acute respiratory complaints for generalist healthcare providers practicing in LMICs. Our goal is to implement this curriculum in the small LMIC of Belize. This module focuses on common respiratory complaints, including asthma, bronchiolitis, pneumonia and acute airway management.
Pulmonary Arteriovenous Malformation in a Patient with Suspected Hereditary Hemorrhagic Telangiectasia: A Case Report
DOI: https://doi.org/10.21980/J8M353Initial vital signs were unremarkable, including oxygen saturation of 98% on room air. The patient did not exhibit any signs of respiratory distress, and the lungs were clear to auscultation bilaterally. Labs were obtained, which showed normal hemoglobin at 15.8. Computed tomography (CT) of the chest (Video 1) showed a large left upper lobe arteriovenous malformation (AVM) with large feeding arteries and tortuous dilated draining veins (red arrow) measuring up to 3.8cm. Imaging also demonstrated nonspecific multifocal ground-glass opacities, which may have represented pulmonary hemorrhage (blue outline) from AVM without evidence of contrast extravasation to suggest active bleeding.
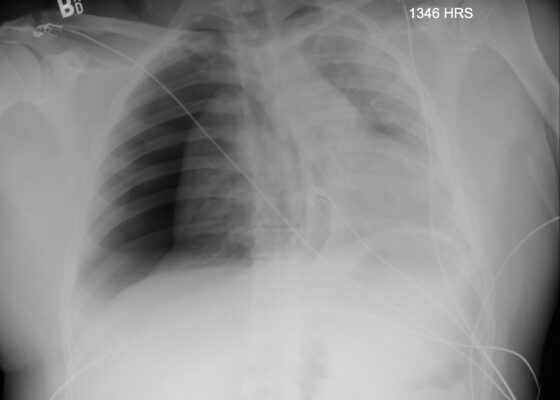
Case Report: Traumatic Tension Pneumothorax in a Pediatric Patient
DOI: https://doi.org/10.21980/J8ZD1SChest X-ray demonstrated significant right-sided pneumothorax (with red outline showing border of collapsed right lung) with cardio mediastinal shift to the left (shown by blue arrows) indicative of a tension pneumothorax
Hemoptysis Due to Diffuse Alveolar Hemorrhage
DOI: https://doi.org/10.21980/J8ZP86By the end of this simulation session, learners will be able to: (1) recognize worsening respiratory status of a patient with hemoptysis and intervene appropriately, (2) manage a patient with severe hemoptysis and perform appropriate ventilator management, (3) manage sinus tachycardia with QT prolongation on the ECG caused by cocaine and hypomagnesemia, (4) address various etiologies of hemoptysis, (5) discuss the causes of massive hemoptysis and management options, and (6) review ventilation strategies in an intubated hypoxic patient.
Improving Emergency Department Airway Preparedness in the Era of COVID-19: An Interprofessional, In Situ Simulation
DOI: https://doi.org/10.21980/J8V06MAt the conclusion of the simulation session, learners will be able to: 1) Understand the need to notify team members of a planned COVID intubation including: physician, respiratory therapist, pharmacist, nurse(s), and ED technician. 2) Distinguish between in-room and out-of-room personnel during high-risk aerosolizing procedures. 3) Distinguish between in-room and out-of-room equipment during high-risk aerosolizing procedures to minimize contamination. 4) Appropriately select oxygenation therapies and avoid high-risk aerosolizing procedures. 5) Manage high risk scenarios such as hypotension or failed intubation and be prepared to give push-dose vasoactive medications or place a rescue device such as an I-gel®.
Low Fidelity Trainer for Fiberoptic Scope Use in the Emergency Department
DOI: https://doi.org/10.21980/J8764BBy the end of this training session, learners will be able to 1) list indications, contraindication, and complications in performing fiberoptic intubations, 2) know how to use and maneuver a fiberoptic scope, and 3) be able to successfully intubate the trainer model.
A Case Report on Miliary Tuberculosis in Acute Immune Reconstitution Inflammatory Syndrome
DOI: https://doi.org/10.21980/J81H02A portable single-view radiograph of the chest was obtained upon the patient’s arrival to the ED resuscitation bay that showed diffuse reticulonodular airspace opacities (red arrows) seen throughout the bilateral lungs, concerning for disseminated pulmonary tuberculosis. Subsequently, a computed tomography (CT) angiography of the chest was obtained which again demonstrates this diffuse reticulonodular airspace opacity pattern (red arrows).
A Just-in-Time Video Primer on Pneumothorax Pathophysiology and Early Management
DOI: https://doi.org/10.21980/J8891JBy the end of this module, participants should be able to: 1) review the normal physiology of the pleural space; 2) discuss the pathophysiology of pneumothorax; 3) describe the clinical presentation of pneumothorax; 4) identify pneumothorax on a chest radiograph; and 5) review treatment options for pneumothorax.