Respiratory
Telemedicine Consult for Shortness of Breath Due to Sympathetic Crashing Acute Pulmonary Edema
DOI: https://doi.org/10.21980/J8HS86At the completion of the simulation and debriefing, the learner will be able to: 1) recognize the physical exam findings and presentation of SCAPE, 2) utilize imaging and laboratory results to further aid in the diagnosis of SCAPE, 3) initiate treatments necessary for the stabilization of SCAPE, 4) demonstrate the ability to assist with the stabilization and disposition of a patient via tele-medicine as determined by the critical action checklist and assessment tool below, 5) interpret the electrocardiogram (EKG) as atrial fibrillation with rapid ventricular response (AFRVR), and 6) recognize that SCAPE is the underlying cause of AFRVR and continue to treat the former.
Electronic Cigarette or Vaping-Associated Lung Injury Case Report
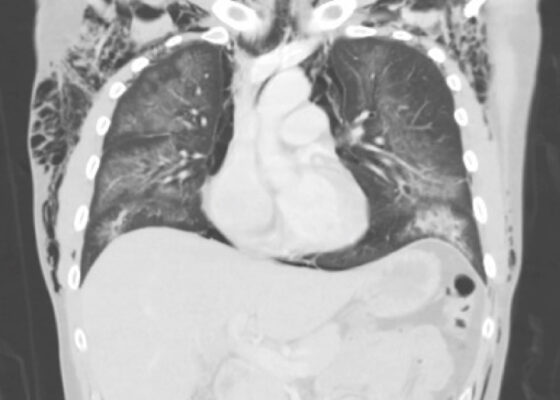
DOI: https://doi.org/10.21980/J8S65PThe CT of the chest with contrast showed subcutaneous emphysema (green star), pneumomediastinum (yellow arrow), and pneumopericardium (purple asterix) without an identifiable tracheal tear. Extensive air was visualized as hypodense areas within the chest wall within the soft tissue. The image also detailed a hypodense area surrounding the heart consistent with pneumopericardium. No disruption of the trachea was present. Additionally, the CT of the chest also showed bilateral ground glass airspace opacities (red stars) with subpleural sparing that is consistent with EVALI findings.2,5 These specific findings have been seen in many of the EVALI cases.5 This image is interesting because there is extensive pneumomediastinum with no clearly identifiable cause. The imaging shows no esophageal or tracheal or lung injury, so it is important to note relevant information collected during interview regarding patient’s recent history of vaping THC, especially when establishing a differential diagnosis.
Respiratory Distress in the Pediatric ED: A Case-based Self-directed Learning Module
DOI: https://doi.org/10.21980/J8T64MEducational Objectives: By the end of this module, learners will be able to: 1) recognize the unique pathophysiology for respiratory distress in the pediatric population and formulate a broad differential; 2) understand the treatment principles for the most common causes of respiratory distress in children; 3) navigate and apply validated clinical decision-making tools for treatment of pediatric respiratory illnesses.
Zombie Cruise Ship Virtual Escape Room for POCUS Pulmonary: Scan Your Way Out
DOI: https://doi.org/10.21980/J8RM0MBy the end of performing the Zombie Cruise Ship Virtual Escape Room, learners will be able to: 1) recognize sonographic signs of A-line, B-line, Barcode sign, Bat sign, Seashore Sign, Plankton sign, Jellyfish Sign, Lung point, lung lockets, and Lung pulse; 2) differentiate sonographic findings of pneumothorax, hemothorax, pneumonia, COVID 19 pneumonia, pulmonary edema, and pleural effusion from normal lung findings; 3) distinguish pneumonia from atelectasis by recognizing dynamic air bronchogram; and 4) recognize indications for performing POCUS pulmonary such as dyspnea, blunt trauma, fall, cough and/or heart failure.
Case Report of an Empyema Identified on Lung Ultrasound
DOI: https://doi.org/10.21980/J8SH2NUsing a curvilinear ultrasound probe, images of the patient were obtained from the left mix-axillary line. These images demonstrate a loculated left-sided pleural effusion (outlined in the attached ultrasound image in blue) that was moderate in size, concerning for an empyema. The diaphragm on the right (red) of the image outlines the inferior margin of the collection of pus, which is seen in the inferior aspect of the left lung. Unfortunately, rib shadows on the left side of the image prevent the full empyema from being captured in this single image. As a result of the bedside ultrasound, however, the patient was rapidly diagnosed with an empyema and was initiated on antibiotics, which is further discussed below. After his bedside ultrasound was completed, his chest x-ray revealed the expected left-sided pleural effusion. Additionally, a CT angiogram of the chest was ordered to rule out a pulmonary embolism, which was negative for an embolism but does redemonstrate the left-sided loculated pleural effusion (outlined on the CT axial and coronal images in blue).
Modified Manikin for Tracheoinnominate Artery Fistula
DOI: https://doi.org/10.21980/J8Z93HBy the end of this educational session, learners will be able to: 1) perform a focused history and physical exam on any patient who presents with bleeding from the tracheostomy site; 2) describe the differential diagnosis of bleeding from a tracheostomy site, including a TIAF; 3) demonstrate the stepwise management of bleeding from a suspected TIAF, including cuff hyperinflation and the Utley Maneuver; 4) verify that definitive airway control via endotracheal intubation is only feasible in the tracheostomy patient when it is clear, upon history and exam, that the patient can be intubated from above; and 5) demonstrate additional critical actions in the management of a patient with a TIAF, including early consultation with otolaryngology and cardiothoracic surgery as well as emergent blood transfusion and activation of a massive transfusion protocol.
Tracheoinnominate Artery Fistula
DOI: https://doi.org/10.21980/J8K05RBy the end of this simulation, learners will be able to: 1) perform a focused history and physical exam on any patient who presents with bleeding from the tracheostomy site, 2) describe the differential diagnosis of bleeding from a tracheostomy site, including a TIAF, 3) demonstrate the stepwise management of bleeding from a suspected TIAF, including cuff hyperinflation and the Utley Maneuver, 4) verify that definitive airway control via endotracheal intubation is only feasible in the tracheostomy patient when it is clear, upon history and exam, that the patient can be intubated from above, 5) demonstrate additional critical actions in the management of a patient with a TIAF, including early consultation with otolaryngology and cardiothoracic surgery as well as emergent blood transfusion and activation of a massive transfusion protocol.
A Pediatric Emergency Medicine Refresher Course for Generalist Healthcare Providers in Belize: Respiratory Emergencies
DOI: https://doi.org/10.21980/J84063This curriculum presents a refresher course in recognizing and stabilizing pediatric acute respiratory complaints for generalist healthcare providers practicing in LMICs. Our goal is to implement this curriculum in the small LMIC of Belize. This module focuses on common respiratory complaints, including asthma, bronchiolitis, pneumonia and acute airway management.