Ob/Gyn
Fitz Hugh Curtis Case Report
DOI: https://doi.org/10.21980/J82K9GA sagittal view from computed tomography (CT) of the abdomen and pelvis demonstrated fat stranding beneath the inferior margin of the liver (outlined in red). The axial view showed fat stranding adjacent to the ascending colon without significant colon wall thickening (arrow). Fat stranding can occur as a hazy increased attenuation (brightness) or a more distinct reticular pattern.
Post-Termination Hemorrhage
DOI: https://doi.org/10.21980/J8NW6QBy the end of this simulation, participants will be able to: 1) recognize post-termination hemorrhage and hemorrhagic shock; 2) demonstrate appropriate acute resuscitation for a patient with hemorrhagic shock; 3) review the differential diagnosis for a patient with post-termination hemorrhage; 4) identify the indications for massive transfusion protocol.
The Gravid Watermelon: An Inexpensive Perimortem Caesarean Section Model
DOI: https://doi.org/10.21980/J8705NThe gravid watermelon is a cost-effective model that uses common materials from the supermarket and emergency department (ED), using a carved-out watermelon as a base, representing the peritoneal cavity. Inexpensive respiratory tubing is used to represent intestine; watered down gelatin and a small doll in a deflated rubber/plastic ball is used to represent a gravid uterus. The bladder is represented by an unused, water-filled exam glove, and watermelon pulp represents blood clots and mesentery. The gravid watermelon is covered with an elastic bandage to represent tough muscle and fascia, and topped with a shower curtain for skin.
Ovarian Teratoma
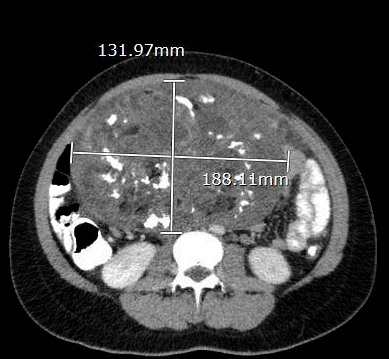
DOI: https://doi.org/10.21980/J8934XThe CT scan with oral contrast in the emergency department revealed a large heterogeneous abdominopelvic mass measuring 13.2 x 18.8 x 23.1 cm (see white lines), suggestive of an ovarian teratoma from the right ovary. This mass included fat, fluid, calcifications (see yellow arrows), and enhancing soft tissue components. The teratoma resulted in mass effect upon large and small bowel loops (see blue highlighted areas), inferior vena cava (IVC), distal aorta (see red highlighted area) and right common iliac artery. A small volume of ascites was also observed. There was no evidence of bowel obstruction, vascular occlusion or other significant emergent finding. Additionally, transabdominal and transvaginal ultrasound images were obtained. The transabdominal image visualized the abdominopelvic mass (see four yellow stars). The transvaginal image visualized a cross section of the teratoma (see four red stars) in relation to the bladder (see four blue stars).
Point-of-care Ultrasound for the Diagnosis of Ovarian and Fallopian Tube Torsion
DOI: https://doi.org/10.21980/J8D06KThe ultrasound video clip demonstrates a transverse view of the pelvis using the endocavitary probe. The bladder can be seen on the anterior portion of the scan (yellow arrow), while the uterus with an intrauterine pregnancy is visible posteriorly (blue arrow). The thickened appearance of the uterine wall is also indicative of pregnancy. A large, anechoic cystic structure measuring approximately 5 cm is seen in the vicinity of the patient’s left adnexa (pink arrow), which raises concerns for ovarian torsion.
A Rare Cause of Pelvic Pain in a Teenage Girl
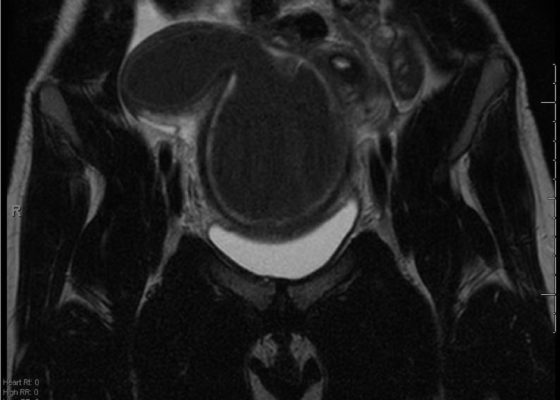
DOI: https://doi.org/10.21980/J87D0WDue to pain out of proportion to her exam, an ultrasound of her pelvis was obtained and showed a blood-filled distended uterus, or hematometrocolpos (white arrow), with a 4.9 cm right ovarian cyst (blue arrow). A pelvic magnetic resonance imaging (MRI) then revealed an obstructed right hemi-vagina, normal left uterus and vagina and ipsilateral renal agenesis (red arrow) with normal left kidney (double arrow) consistent with obstructed hemivagina, ipsilateral renal agenesis (OHVIRA) syndrome. The patient underwent surgical repair with complete resolution of symptoms.