Neurology
Headache Over Heels: CT Negative Subarachnoid Hemorrhage
DOI: https://doi.org/10.21980/J8ND2CBy the end of this case, the participant will be able to: 1) construct a broad differential diagnosis for a patient presenting with syncope, 2) name the history and physical exam findings consistent with SAH, 3) identify SAH on computer tomography (CT) imaging, 4) identify the need for lumbar puncture (LP) to diagnose SAH when CT head is non-diagnostic > 6 hours after symptom onset, 5) correctly interpret cerebral fluid studies (CSF) to aid in the diagnosis of SAH, and 6) specify blood pressure goals in SAH and suggest appropriate medication management.
Epilepsy Caused by Neurocysticercosis: A Case Report
DOI: https://doi.org/10.21980/J81P96In our patient, two lesions were most notable on CT in the frontal and occipital lobes. The lesion in the left frontal lobe (blue circle) was an approximately 1.5 centimeter (cm) rounded area with rim enhancement and surrounding hypodensity, consistent with vasogenic edema. A similar sized low-density area in the left occipital lobe (red circle) was noted, with increased peripheral density at the 3 o’clock position representing calcification. There were no areas of apparent hemorrhage or midline shift. The final radiology report concluded there were multiple cystic lesions, one with surrounding vasogenic edema in the left frontal lobe.
A Case Report of a Man with Burning Arm and Leg Weakness
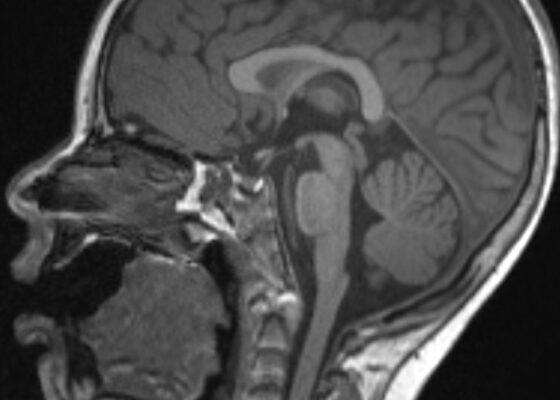
DOI: https://doi.org/10.21980/J8V659A non-contrast computed tomography (CT) of the head and neck was performed, followed by an MRI of the cervical spine. The CT demonstrated congenital narrowing of the cervical spinal canal, with posterior disc osteophyte complex and disc bulge at C3-4 and C4-5 (arrow). The T2-weighted MRI additionally demonstrated obliteration of the anterior and posterior subarachnoid space at the level of C3-C5, with associated patchy central cord signal abnormality (arrow).
Transverse Myelitis in Naloxone Reversible Acute Respiratory Failure—A Case Report
DOI: https://doi.org/10.21980/J8B659Magnetic resonance imaging of the brain, cervical, thoracic and lumbar spine without contrast was obtained and revealed increased signal throughout the spinal cord from C-1 to the conus medullaris with mild expansion consistent with transverse myelitis.
An Unusual Case Report of a Toddler with Metastatic Neuroblastoma Mimicking Myasthenia Gravis
DOI: https://doi.org/10.21980/J8G35VWhile still in the ED, MRI with and without gadolinium contrast of the brain, orbits, and cervical, thoracic and lumbar spine were obtained to evaluate for possible CNS lesions including encephalitis, myelitis, or demyelination. Imaging, however, demonstrated multiple unexpected findings: a T1 hypointense, T2 hyperintense and heterogeneously enhancing right adrenal mass measuring 2.7 x 2.1 x 3 cm (yellow asterisk) along with heterogenous enhancement at the clivus, C6, C7, T7, T8, T12, and L3 vertebral bodies (red asterisks). There were otherwise no significant intracranial signal or structural abnormalities and normal orbits.
Case Report of a Man with Right Eye Pain and Double Vision
DOI: https://doi.org/10.21980/J8KW7GABSTRACT: A 39-year-old previously healthy male presented with three days of right eye pressure and one day of binocular diplopia. He denied history of trauma, headache, or other neurological complaints. He had normal visual acuity, normal intraocular pressure, intact convergence, and no afferent pupillary defect. His neurologic examination was non-focal except for an inability to adduct the right eye past midline
Meningococcal Meningitis with Waterhouse-Friderichsen Syndrome
DOI: https://doi.org/10.21980/J8TH1KBy the end of this simulation session, learners will be able to: (1) manage a patient with altered mental status (AMS) with fever while maintaining a broad differential diagnosis, (2) recognize the risk factors for meningococcal meningitis, (3) manage a patient with worsening shock and perform appropriate resuscitation, (4) develop a differential diagnosis for thrombocytopenia and elevated international normalized ratio (INR) in an altered febrile hypotensive patient with rash, (5) manage the bleeding complications from WFS, (6) discuss the complications of meningococcal meningitis including WFS, and (7) review when meningitis prophylaxis is given.