Cardiology/Vascular
Saddle Pulmonary Embolus
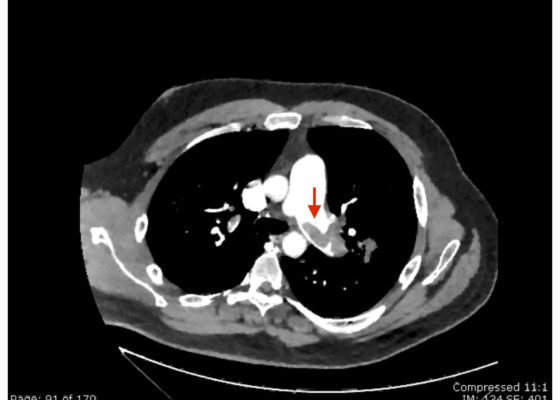
DOI: https://doi.org/10.21980/J8N63PAn electrocardiogram (ECG) showed evidence of right heart strain with an incomplete right bundle branch block, S1Q3T3 (see red arrow [S1], blue arrow [Q3], and black arrow [T3]), and ST-segment elevation in the septal leads (green arrows). Bedside echocardiography showed a dilated right ventricle with ventricular wall akinesis (red arrow) sparing the apex (purple arrow), which is known as McConnell’s Sign. It also showed a mobile hyperechoic mass (yellow arrow). These ultrasound findings were concerning for pulmonary embolism (PE), so computed tomography (CT) angiogram of the chest was ordered and confirmed massive bilateral obstructive filling defects (red arrows) consistent with saddle pulmonary embolism. Additionally, noted is flattening of the interventricular septum (blue arrow) consistent with right heart strain. Laboratory studies were notable for a troponin-I of 0.29 ng/mL, a B-type natriuretic peptide of 792.3 pg/mL, lactic acid of 5.30 mmol/L, and a creatinine of 2.0 mg/dL, consistent with end organ dysfunction. All other lab work was within normal limits.
Pericardial Clot on Point-of-Care Ultrasound
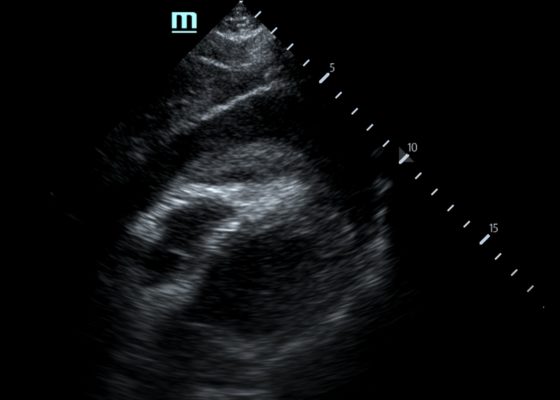
DOI: https://doi.org/10.21980/J8ZH1TFocused assessment with sonography in trauma (FAST) scan was positive for a clinically significant pericardial effusion as evidenced by the hypoechoic fluid around the myocardium, indicated by the blue arrow in image 2. Findings are also consistent with tamponade process as evidenced by restricted expansion and collapse of the right ventricle during diastole. The hyperechoic floating structure between the pericardium and myocardium, adjacent to the right ventricle, represents a pericardial clot, indicated by the white arrow.The density of the pericardial clot differs from that of the myocardium, thus serving as an additional variable to avoid confusing this as part of the myocardial structure.
Wellens’ Syndrome
DOI: https://doi.org/10.21980/J8FS8KInitial electrocardiogram (ECG) revealed the classic biphasic T waves in V2 and V3 of Wellen’s syndrome (see red outlines). A second EKG demonstrated an evolving deeply inverted T wave (see blue outlines).
Arteriovenous Graft Pseudoaneurysm
DOI: https://doi.org/10.21980/J8B06ZA bedside ultrasound of the mass demonstrated a large compressible hypoechoic structure (see purple outline) above the arteriovenous graft (see red outline). The contents demonstrated movement of fluid within the structure. This was confirmed with Doppler mode, which allowed for visualization of flow communicating between the structure and the underlying vessel, which is diagnostic for a pseudoaneurysm.
Guilty as Charged: Jailed Coronary Vessel Presenting as Wellens’ Syndrome Type B
DOI: https://doi.org/10.21980/J8DS6HEvolving changes to electrocardiograph (ECG) were noted during serial ECG monitoring involving leads V2 and V3, along with some T-wave inversion in V4 and V5 that were concerning for a Wellens’ syndrome type B on second ECG. She was admitted and subsequently taken to cardiac catheterization suite where it was revealed that the previously placed stent in the left anterior descending (LAD) artery was patent. Unfortunately, the stent blocked off an adjacent side branch vessel off the LAD in proximal two-third region of the stent (as seen in the cartoon).
Intramural Hematoma with Type B Aortic Dissection
DOI: https://doi.org/10.21980/J81M03Computed tomography angiography of the chest and abdomen revealed a 9.5 cm thoracoabdominal aneurysm (red outline) with intramural hematoma (yellow shading) and large left pleural effusion versus hemothorax with old blood (blue shading).
Cocaine-induced Myocardial Infarction and Pulmonary Edema
DOI: https://doi.org/10.21980/J8ZS87By the end of this simulation session, the learners will be able to:1) Determine appropriate diagnostics in a patient with likely cocaine toxicity. 2) Identify and manage respiratory failure. 3) Identify and manage a ST-elevation myocardial infarction (STEMI) and pulmonary edema. 4) Identify and manage cocaine toxicity with benzodiazepines. 5) Determine appropriate disposition of the patient to the cardiac catheterization lab and an intensive care unit (ICU). 6) Demonstrate effective communication and teamwork during resuscitation of a critically ill patient.
Prehospital Cardiac Arrest Management Simulation
DOI: https://doi.org/10.21980/J8V057At the end of this simulation learners will be able to: 1) Perform team-focused CPR using effective leadership and communication skills during prehospital resuscitation. 2) Employ high-quality CPR with an emphasis on compressions and early defibrillation. 3) Demonstrate appropriate airway management utilizing an oropharyngeal airway and bag-valve-mask, blind-insertion airway device, and/or endotracheal intubation during cardiac arrest. 4) Recognize and appropriately defibrillate pulseless ventricular tachycardia and ventricular fibrillation. 5) Formulate an appropriate differential diagnosis for pulseless electrical activity.