Rare Rapidly Growing Thumb Lesion in a 12-Year-Old Male
History of present illness:
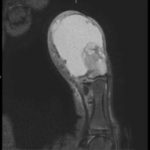
A 12-year-old male presented to the emergency department with right thumb pain and a mass for four months (see images). He denied fevers, chills, change in appetite, or fatigue. He noted that the lesion was growing and “bleeds easily if bumped.” He denied any trauma to the thumb, except “hitting it” months ago while in football practice.
Workup in the ED included complete blood cell count (CBC), comprehensive metabolic panel (CMP), erythrocyte sedimentation rate (ESR), coagulation studies, uric acid, and lactic dehydrogenase (LDH), all of which were within normal limits.
Significant findings:
Magnetic resonance imaging (MRI) showed an “expansile, destructive solid and cystic mass with aggressive…characteristics…” (see images). Tissue biopsy confirmed a giant cell tumor arising from the bone. The patient underwent a debulking procedure, and later a distal amputation. Follow-up on pathology showed negative margins.
Discussion:
Giant cell tumor of the bone (GCTB)is a rare, often benign but locally aggressive neoplasm creating osteolytic lesions, commonly affecting long bones.Overall incidence is approximately one person per million per year.1,2 Pain is the leading symptom at presentation. Depending on the duration of disease, a mass may be present. Often, around joint involvement, there is a mechanical deficiency and poor strength due to local cortical disruption of the bone.3
In 80% of cases, the course of GCTB is benign; however, local recurrence rate is 20%–50%.4 Approximately 10% of tumors undergo malignant transformation during recurrence, and 1%–4% give rise to pulmonary metastases even in cases of benign histology.4 GCTB occurs most commonly during the second to fourth decades of life (60%–75%).5 The majority of lesions develop in the long bones (75%–90%), with most cases (50%–65%) occurring near the knee.5 Most complications arise if there are pulmonary metastases. Radiation and chemotherapy can be used in those cases that aren’t amenable to surgery.4
Surgery is the mainstay of care. The first medical treatment, denosumab, was approved by the FDA for use in adults and skeletally mature adolescents with surgically unresectable lesions.5 It is critical to obtain definitive imaging and biopsy of any rapidly growing lesions in patients presenting with masses and no history of trauma or constitutional symptoms.
The best imaging study is MRI, to assess for bony and tissue involvement and surgical approach. Computed tomography may be used; however, it doesn’t delineate the soft tissue and bony connections as well. Standard oncology labs should be drawn as well, including: CBC with differential, LDH, uric acid, CMP, ESR. The growth of the tumor is insidious and therefore imaging should be done based on clinical concern. In the ED setting, if close follow up can be ensured, imaging can be done as an out-patient. Annual surveillance is recommended for at least five years in most patients, even after total resection, according to some studies.3
Our patient underwent GCTB resection with plastics surgery of the distal phalanx of thumb. He was seen in follow-up in the oncology clinic. Pathology of the tumor had negative margins, and he was told to follow-up in six months with plastics. Per hematology, no further follow-up was needed.
Topics:
Pediatrics, giant cell tumor, thumb lesion.
References:
- Larsson SE, Lorentzon R, Boquist L. Giant-cell tumor of bone. A demographic, clinical, and histopathological study of all cases recorded in the Swedish Cancer Registry for the years 1958 through 1968. J Bone Joint Surg Am. 1975;57(2):167-73.
- Liede A, Bach BA, Stryker S,et al. Regional variation and challenges in estimating the incidence of giant cell tumor of bone. J Bone Joint Surg. 2014;96(23):1999-2007. doi: 10.2106/JBJS.N.00367.
- Klenke FM, Wenger DE, Inwards CY, Rose PS, Sin FH. Giant cell tumor of bone: risk factors for recurrence. Clin Ortop Relat Res. 2011;469(2):591-599. doi: 10.1007/s11999-010-1501-7
- Yelin E, Weinstein S, King T. The burden of musculoskeletal diseases in the United States. 2nd ed. Semin Arthirtis Rheum. 2016;46(3):259-260. doi: 10.1016/j.semarthrit.2016.07.013
- Xu SF, Adams B, Yu XC, Xu M. Denosumab and giant cell tumour of bone-a review and future management considerations. Curr Oncol. 2013;20(5):e442-447. doi: 10.3747/co.20.1497
- Thomas DM, Skubitz KM.Giant cell tumour of bone. Curr Opin Oncol. 2009;2(4):338-44.doi: 10.1097/CCO.0b013e32832c951d