CT
The Elusive Pheo: A Case Report of Pheochromocytoma in the Emergency Department
DOI: https://doi.org/10.21980/J8KW63ED work-up: BMP within normal limits (WNL), white blood cell (WBC) 27.4, ECG showed sinus tachycardia, nonspecific ST segment abnormalities, BNP and troponin were within normal limits, HR 146 beats/minute, CT abdomen/pelvis showed a 10-cm-heterogenous enhancing left adrenal mass (anterior-posterior view [shown in red], lateral view [shown in blue]).
Traumatic Diaphragmatic Rupture – A Case Report
DOI: https://doi.org/10.21980/J8G64HChest X-ray showed an elevated left hemi-diaphragm with superior displacement of a portion of intra-abdominal contents presumed to be the stomach (green arrowheads) with associated rightward mediastinal shift (yellow arrows). The diagnosis was confirmed by CT. Computed tomography imaging of the chest showed a large, left diaphragmatic defect measuring approximately 5.5 cm with herniation of the upper half of the stomach through the defect. The fundus of the stomach (blue arrow) herniated superiorly through the ruptured diaphragm (red arrow).
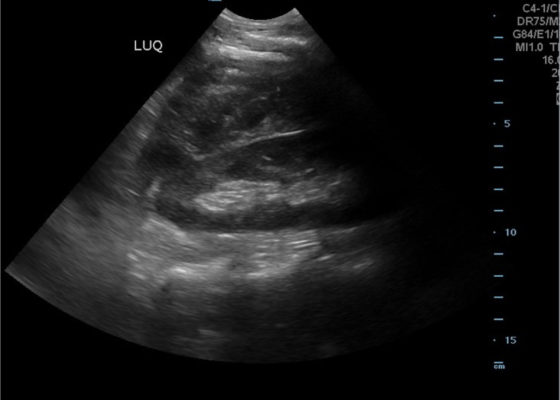
FAST Exam to Diagnose Subcapsular Renal Hematoma
DOI: https://doi.org/10.21980/J8NP8DA bedside point of care ultrasound FAST exam was performed revealing a left subcapsular renal hematoma. The hematoma was a non-compressing hematoma, evidenced by preserved renal contour with the hematoma labeled with a red H and the normal renal contour labeled with a green K. Additionally, cortical necrosis and ischemia can be characterized by a dark, hypoechogenic renal cortex on ultrasonography with a decrease in flow to the cortex on color doppler which was not seen on this patient, providing further evidence that the hematoma was non-compressing. The hematoma was concluded to be an acute process due to its hypoechoic appearance with some mixed ultrasonographic echoes caused by the early deposit of fibrin.
Right Upper Quadrant Pain in a World Explorer
DOI: https://doi.org/10.21980/J8QP9DThe ultrasound images show the abscess, which is a large, circular, hypoechoic mass outlined in blue in the center of the image. The abscess is surrounded by the hyperechoic and heterogeneous liver tissue.
For better delineation of the abscess, a CT was ordered. The axial CT scan image shows the liver abscess, which appears as a hypodense, ovoid, intrahepatic fluid collection within the liver parenchyma. The size of the abscess has been annotated with a dotted line measuring 194.9 mm x 166.2 mm.
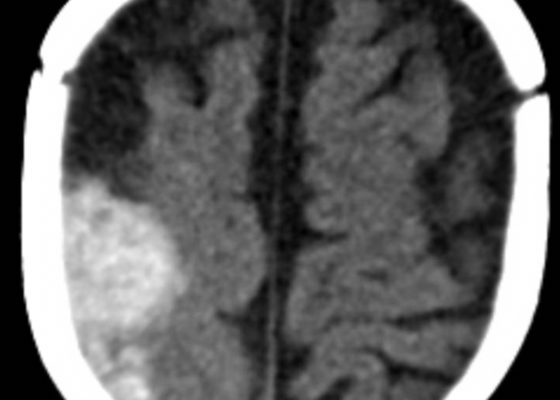
Spontaneous Intracranial Hemorrhage in Severe Hemophilia A: A Rare Cause of Seizure in a Young Child
DOI: https://doi.org/10.21980/J8G91DA computed tomography (CT) scan of the head without contrast was obtained out of concern for intracranial pathology due to the patient’s young age and the witnessed focal seizure. The CT showed a 4.2 x 1.2 x 1.5 cm acute extra-axial intracranial right frontoparietal hemorrhage favoring epidural over subdural hemorrhage given its lenticular shape. There was no underlying fracture, herniation or midline shift identified.
Gastric Volvulus
DOI: https://doi.org/10.21980/J8335FPoint of care ultrasound of his abdomen showed a large fluid filled structure with well-defined borders containing gastric contents extending from the xiphoid process to the umbilical region. No free fluid was noted on focus assessment with sonography for trauma (FAST) examination. A computed tomography (CT) scan was performed emergently and it was noted that the patient had a significantly distended stomach and gastric volvulus (blue arrows) noted in the area of his paraesophageal/hiatal hernia.
Wandering Spleen
DOI: https://doi.org/10.21980/J8PS7CHistory of present illness: A 7-month-old boy presented for evaluation of an abdominal mass. Two weeks prior, the patient had a fever followed by 24 hours of vomiting and abdominal pain, which self-resolved. His pediatrician noted the mass on exam and referred child to the emergency department (ED). His abdominal exam was significant for a hard mass palpated to the
Acute Pancreatitis
DOI: https://doi.org/10.21980/J88W5XComputed tomography of the abdomen and pelvis with contrast show edema of the pancreas (red outline) and duodenum (yellow arrow) with peripancreatic inflammation, fluid and fat stranding (blue highlight). The distal pancreatic tail was noted to appear normal (green arrow). There was no organized drainable fluid collection, and no parenchymal hypo-enhancement. These findings are consistent with moderate severity acute interstitial pancreatitis.