Sialadenitis
History of present illness:
The patient is a 15-year-old male who presented to the emergency department with right-sided submandibular swelling that started three days prior to arrival. He noted worsening of symptoms on the day of presentation with dysphagia and odynophagia. He described a subjective fever, rhinorrhea, and a non-productive cough at onset of symptoms that resolved.
Significant findings:
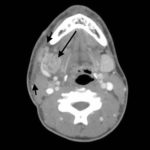
The computed tomography (CT) scan demonstrates prominent enlargement and heterogeneous enhancement of the right submandibular gland (single large arrow) compatible with sialadenitis. There is no evidence of a sialolith or obstruction on the CT. There is associated edema (two small arrows) of the right submandibular space, parapharyngeal space and anterior right neck with partial effacement of the right vallecula and right pyriform sinus.
Discussion:
The patient has sialadenitis, which is an infection of the salivary gland caused by either a bacteria or virus. Staphylococcus aureus is the most common cause, but Streptococcus pneumoniae, viridans streptococci, and Haemophilus influenzae are also possible etiologies.1 The infection occurs in the submandibular gland 80%-92% of the time. The second most common site is the parotid gland.2 The presentation is almost always unilateral. Symptoms typically include sudden onset of swelling of the involved gland. Fever and chills can also be present.2 Risk factors for sialadenitis include: sialolithiasis, dehydration, Sjögren syndrome, connective tissue disease, and periodontal disease.3
Computed tomography is ten-fold more sensitive at detecting sialoliths and sialadenitis when compared to plain films. Patients with sialadenitis are typically managed in an outpatient setting with antibiotics and analgesia. Dicloxacillin and cephalexin are commonly used antibiotics. Non-steroidal anti-inflammatory drugs (NSAIDs) are recommended for analgesia. Sialolithiasis is a leading cause of sialadenitis and occurs when a salivary stone gets wedged in the salivary duct, which can then lead to infection of the gland behind the obstruction. If a sialolith is present, lemon drops or any sour lozenge are common sialagogues that can help promote passage of the stone to aid in clearance of the infection. Symptoms typically resolve in 7-10 days.2 If the symptoms do not improve, otolaryngology (ENT) follow up for sialendoscopy is indicated.5
Topics:
Sialadenitis, salivary glands, sialolithiasis.
References:
- Chow A.W Infections of the oral cavity, neck, and head. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 8th Philadelphia, PA: Elsevier; 2015:789-805.
- Pfaff J, Moore GP. Otolaryngology. Walls RM, Hockberger RS, Gausche-Hill M, Bakes KM, eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 9th Philadelphia, PA: Elsevier; 2018:931-940.
- Huoh KC, Eisele DW. Etiologic factors in sialolithiasis. Otolaryngol Head Neck Surg.2011; 145:935. doi: 10.1177/0194599811415489
- Thomas WW, Douglas JE, Rassekh CH. Accuracy of ultrasound and computed tomography in the evaluation of patients undergoing sialendoscopy for sialolithiasis. Otolaryngol Head Neck Surg.2017;156(5):834-839. doi: 10.1177/0194599817686308
- Strychowsky JE, Sommer DD, Gupta MK, Cohen N, Nahlieli O. Sialendoscopy for the management of obstructive salivary gland disease: a systematic review and meta-analysis. Arch Otolaryngol Head Neck Surg.2012; 138:541-547. doi: 10.1001/archoto.2012.856