Ultrasound
Ultrasound Case: Syncope in PE
DOI: https://doi.org/10.21980/J8.52365By the end of the session, learners will be able to: 1) obtain and interpret the parasternal short-axis view of the heart to assess right ventricular size and function, 2) identify ultrasound findings suggestive of pulmonary embolism (PE) on cardiac short-axis view, including right ventricular dilation and septal bowing, 3) demonstrate appropriate probe selection and positioning to obtain optimal images of the heart and inferior vena cava (IVC), 4) evaluate the IVC using a subxiphoid or longitudinal view to assess distension and lack of respiratory collapse as supportive findings for elevated right heart pressures, 5) identify the anatomy of the neck vasculature, differentiate between the internal jugular vein and carotid artery, and select the appropriate puncture site, 6) describe ultrasound-guided central venous catheterization via the right internal jugular vein, using a sterile technique and real-time guidance
In Too Deep: A Point-of-Care Ultrasound (POCUS) Escape Room
DOI: https://doi.org/10.21980/J8.52100By the end of this session, the participant will be able to: 1) evaluate and identify the nature of metallic foreign bodies using POCUS; 2) identify common emergency department fractures on X-Ray and identify relevant sonoanatomy for ultrasound-guided regional anesthesia applications relevant to those fractures; and 3) identify normal lower extremity venous POCUS sonoanatomy and demonstrate understanding of proximal versus distal anatomical location within the lower extremity venous system.
Ultrasound Guided Peripheral Nerve Block Workshop: How to Take Your Residents from Zero to Hero
DOI: https://doi.org/10.21980/J8.52156After completing this small group workshop, the resident should be able to: 1) recognize the indications for the serratus anterior plane block, the posterior tibial block and the ulnar, median, and radial nerve blocks and the anatomical locations that would benefit from these blocks, 2) identify proper probe selection and placement, in addition to patient positioning, in order to perform these blocks, as well as anesthetic choice and dosing, 3) demonstrate knowledge of anatomical landmarks and areas to avoid evidenced by probe placement and positioning, 4) describe the steps to perform these nerve blocks, and 5) demonstrate knowledge of contraindications to these blocks as well as potential complications of these procedures and how to mitigate them.
Innovative Ultrasound-Guided Erector Spinae Plane Nerve Block Model for Training Emergency Medicine Physicians
DOI: https://doi.org/10.21980/J8PW7DThis innovation model is designed to facilitate hands-on training of the ultrasound-guided ESP nerve block using a practical, realistic, and cost-effective ballistics gel model. By the end of this training session, learners should be able to: 1) identify relevant sonoanatomy on the created simulation model; 2) demonstrate proper in-plane technique; and 3) successfully replicate the procedure on a different target on the created training model.
A Case Report of Right Atrial Thrombosis Complicated by Multiple Pulmonary Emboli: POCUS For the Win!
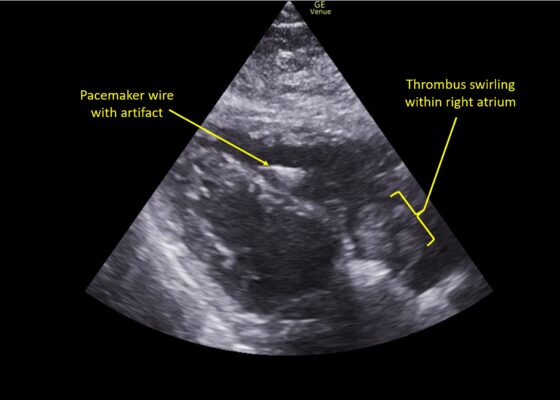
DOI: https://doi.org/10.21980/J8TM07Pulmonary POCUS was performed by the ED physician (GE Venue, C1-5-RS 5MHz curvilinear transducer), and lung examination was unremarkable with no pleural effusion, pneumothorax, or infiltrate. Subxiphoid views (GE Venue, 3Sc-RS 4MHz phased-array transducer) were obtained because this patient’s COPD with severe pulmonary hyperexpansion made parasternal and apical 4-chamber views suboptimal. A large thrombus can be seen within the right atrium (movie 1, images 1, 2). This has a serpiginous, rounded appearance and is mobile, appearing to swirl within the right atrium with intermittent extrusion through the tricuspid valve. A pacemaker wire is also visible within the right ventricle as a non-moving, hyperechoic, linear structure with posterior enhancement artifact. Pericardial effusion is not present.
E-FAST Ultrasound Training Curriculum for Prehospital Emergency Medical Service (EMS) Clinicians
DOI: https://doi.org/10.21980/J8S060By the end of these training activities, prehospital EMS learners will be able to demonstrate foundational ultrasound skills in scanning, interpretation, and artifact recognition by identifying pertinent organs and anatomically relevant structures for an E-FAST examination. Learners will differentiate between normal and pathologic E-FAST ultrasound images by identifying the presence of free fluid and lung sliding. Learners will also explain the clinical significance and application of detecting free fluid during an E-FAST scan.
Point-Of-Care Ultrasound Use for Detection of Multiple Metallic Foreign Body Ingestion in the Pediatric Emergency Department: A Case Report
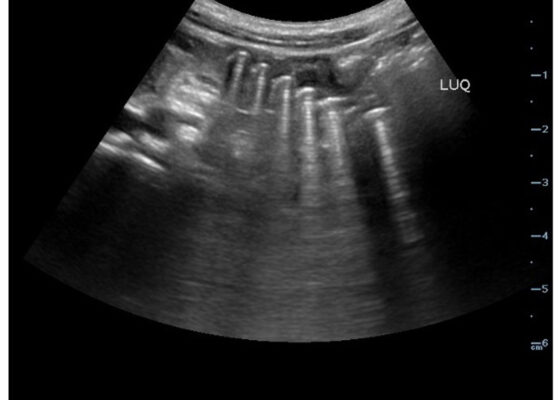
DOI: https://doi.org/10.21980/J83D2DBedside POCUS was performed on the patient’s abdomen using the curvilinear probe. The left upper quadrant POCUS image demonstrates multiple hyperechoic spherical objects with shadowing and reverberation artifacts concerning multiple foreign body ingestions. Though the patient and mother initially denied knowledge of foreign body ingestion, on repeated questioning after POCUS findings, the patient admitted to his mother that he ate the spherical magnets he received for his birthday about one week ago. The patient swallowed these over the course of two days. The presence of multiple radiopaque foreign bodies was confirmed with an abdominal X-ray.
Sonographic Retrobulbar Spot Sign in Diagnosis of Central Retinal Artery Occlusion: A Case Report
DOI: https://doi.org/10.21980/J8735PThe bedside ocular ultrasound (B-scan) was significant for small, hyperechoic signal (white arrow) in the distal aspect of the optic nerve, concerning for embolus in the central retinal artery. Subsequent direct fundoscopic exam was significant for a pale macula with cherry red spot (black arrow), consistent with central retinal artery occlusion (CRAO).