Respiratory
An Innovative Inexpensive Portable Pulmonary Edema Intubation Simulator
DOI: https://doi.org/10.21980/J8MM1RBy the end of the session, learners will be able to: 1. Discuss the pathophysiology of, and immediate stabilization management steps for, acute cardiogenic pulmonary edema. 2. List the indications, contraindications, and risks associated with intubating a patient with acute cardiogenic pulmonary edema. 3. Demonstrate effective communication and teamwork skills to manage the airway of a simulated patient in respiratory distress due to acute cardiogenic pulmonary edema. 4. Successfully and safely intubate a simulated patient with a difficult airway due to visual obstruction from frothy pulmonary edema secretions.
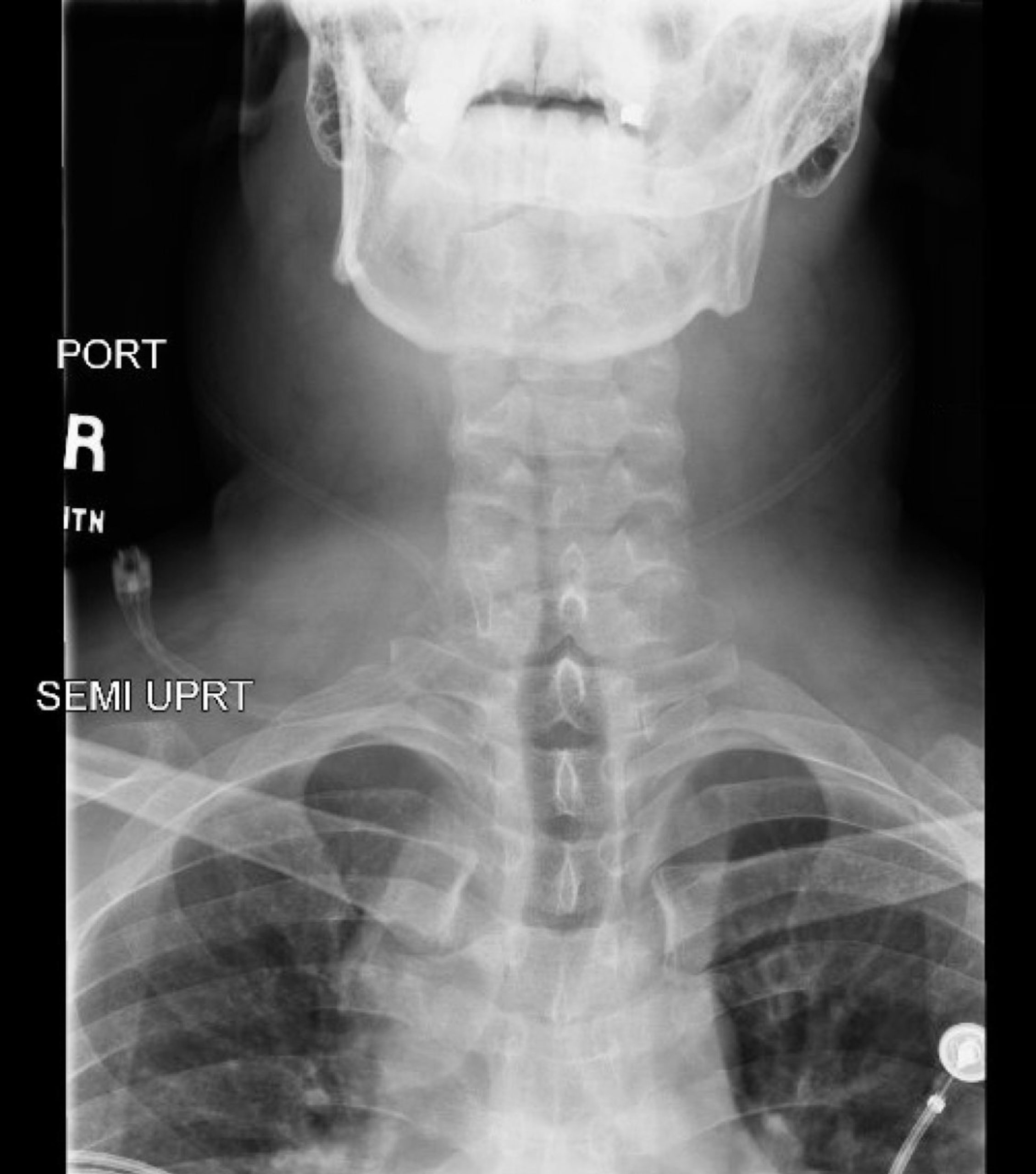
Rapid Airway Narrowing Associated with Hodgkin’s Lymphoma
DOI: https://doi.org/10.21980/J86D3QNeck X-ray showed nonspecific significant prevertebral soft tissue swelling at the level of the cervical spine, with associated apparent thickening of the epiglottis (yellow arrow), diffuse soft tissue swelling of the neck (red arrows) and tracheal airway narrowing (light blue arrow). The computed tomography imaging of the neck was significant for multiple conglomerating pathological lymph nodes with a significant mass effect (orange arrows) compressing the right internal jugular vein (green arrow).
Pulseless Electrical Activity Cardiac Arrest
DOI: https://doi.org/10.21980/J8Z055After competing this simulation-based session, the learner will be able to: 1) Identify PEA arrest; 2) review the ACLS commonly recognized PEA arrest etiologies via the H &T mnemonic; 3) review and discuss the risks and benefits of tissue plasminogen activator (tPA) for massive PE.
A Comprehensive Course for Teaching Emergency Cricothyrotomy
DOI: https://doi.org/10.21980/J8JS9WAfter completing this activity, the learner will be able to: 1) correctly describe the indications for and contraindications to emergency cricothyrotomy; 2) correctly describe and identify on the simulator the anatomic landmarks involved in emergency cricothyrotomy; 3) correctly list the required equipment and the sequence of the steps for the “standard” and “minimalist” variations of the procedure; 4) demonstrate proper technique when performing a cricothyrotomy on the simulator without prompts or pauses.
Case Report of the Unusual Presentation of Stridor in an Elderly Patient Following a Cervical Fracture
DOI: https://doi.org/10.21980/J8V926The cervical CT was significant for a transverse fracture through the C4 vertebral body (see red arrow), lateral facet (green arrow), spinous process (blue arrow), and right lamina (purple arrow) as well as surrounding edema and retropharyngeal thickening (yellow line), best appreciated on sagittal view.
Status Asthmaticus
DOI: https://doi.org/10.21980/J8JW6SAt the end of this case, the learners should be able to diagnose an asthma exacerbation, provide the appropriate medications, determine when intubation is necessary, and describe the general principles of ventilator management in an asthmatic patient.
Emergency Medicine Curriculum Utilizing the Flipped Classroom Method: Pulmonary Emergencies
DOI: https://doi.org/10.21980/J8F646The educational strategies used in this curriculum include small group case-based modules authored by education faculty and content experts based on the core emergency medicine content outlined in the ABEM Model EM curriculum. The Socratic method, used during small group sessions, encourages active participation; small groups also focus on the synthesis and application of knowledge through the discussion of clinical experiences. The use of free open access medical education (FOAM) resources allows learners to work at their own pace and maximize autonomy. Learners are encouraged to use such resources for preparation prior to small group sessions, and also to review and help solidify important points after the conclusion of in-person discussions.
Pneumocystis jirovecii (carinii) Pneumonia
DOI: https://doi.org/10.21980/J8RW6NChest X-ray showed diffuse, patchy interstitial and alveolar infiltrates bilaterally concerning for Pneumocystis jirovecii(previously Pneumocystis carinii) pneumonia (PJP). The AP radiograph (top left figure) showed the classic “bat-wing” distribution on the left side. Repeat radiograph (bottom figure) one day after admission showed worsening of the infiltrates.