Procedures
Pre-Clinical Case Competition to Assess Confidence in Responding to Select Out-Of-Hospital Medical Emergencies
DOI: https://doi.org/10.5070/M5.52198By the end of this activity, learners will be able to: 1) demonstrate the application of skills in real-life first responder scenarios, including suspected opioid overdose, cardiac arrest, and anaphylaxis; 2) apply knowledge of scene safety and the role of the first responder in various situations; and 3) assess the challenges while applying the skills necessary for collaborative work within a medical team.
Pediatric Difficult Airway Simulation Day
DOI: https://doi.org/10.5070/M5.52208The objective of this one-day simulation workshop is to increase learner confidence and skills necessary to perform critical pediatric airway procedures. PEM fellows of all training levels at our institution completed a three-hour “PEM Difficult Airway Day,” which consisted of six 30-minute stations focusing on airway scenarios critical for PEM fellow training: five high- and low-fidelity simulations (premature neonate, inhalational injury, contaminated airway, obese patient, and failed airway) and one discussion-based station on the physiologically difficult intubation. By the end of this workshop, learners will be able to: 1) identify various clinical situations in which a pediatric patient may have a difficult airway, 2) successfully intubate mannequins with simulated difficult airways using direct laryngoscopy (DL), video laryngoscopy (VL), laryngeal mask airway (LMA) placement, bougie-assisted intubation, and a hyper-angulated VL blade, and 3) recognize and describe the management of physiologically difficult airways and failed airways.
A Multimodal Approach to Lateral Canthotomy and Cantholysis Training for Emergency Medicine Trainees: A Simulation Training Package
DOI: https://doi.org/10.5070/M5.52351By the end of this session, learners should be able to: 1) recognize the clinical features of OCS, 2) describe the indications and steps of performing LCC, 3) perform a lateral canthotomy and cantholysis procedure on a low-fidelity model, and 4) demonstrate improved confidence in recognizing and managing OCS.
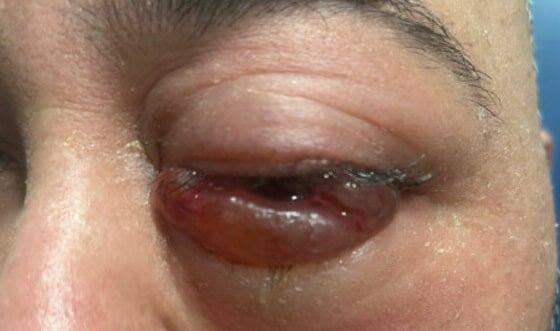
A Case Report of Carotid Cavernous Fistula: A Commonly Missed Diagnosis
DOI: https://doi.org/10.5070/M5.52242The initial physical exam performed by the ED provider revealed severe left eye chemosis, clear drainage, visual acuity of right eye 20/100 and left eye 20/400, and a left eye IOP of 52. There was a deficit of extraocular movement in all directions of gaze and limitation in all visual fields in the left eye. The MRI showed that at the level of the eye, the left cavernous sinus is asymmetrically enlarged compared to the right (red arrow) with an enlarged left inferior petrosal sinus with internal flow void on the pre-contrast MRI images (blue arrow). The orange arrow notes a central filling defect of the left superior ophthalmic vein on the MRA.
Procedural Case: Neonatal Lumbar Puncture
DOI: https://doi.org/10.21980/J8.52364This is a Procedure case involving a neonatal LP. The overarching educational goal of this case is to assess learners’ clinical decision-making, technical proficiency, and communication skills when performing a neonatal LP. Participants will be evaluated on their ability to identify indications and contraindications, obtain informed consent, prepare for and perform the procedure with sterile technique, and implement appropriate post-procedure care. By the end of the session, learners should be able to: 1) describe the indications and contraindications associated with performing a neonatal LP, 2) obtain informed consent for a neonatal LP, using clear, patient-centered language to explain the procedure and to discuss risks, benefits, and alternative options, 3) demonstrate proper preparation for a neonatal LP, including equipment setup, patient positioning, patient monitoring, use of sterile technique, and analgesia, 4) perform a neonatal LP on a procedural task trainer with technical proficiency, demonstrating proper needle insertion, cerebrospinal (CSF) collection, and adherence to sterile technique, and 5) outline appropriate post-procedure management for the patient, including interpreting CSF results, initiating appropriate treatment, monitoring for complications, and providing caregivers with clear follow-up guidance.
A Low-Cost Task Trainer Constructed from Silicone Nipple Covers
DOI: https://doi.org/10.21980/J8.52244Educational Objectives: By the end of this training session, learners will be able to anesthetize an abscess, perform incision and drainage, develop manual dexterity maneuvering instruments to break up the abscess, and place packing using both the linear incision and loop techniques.
Pizza and Paintballs: A Cost-Effective Model for Incision and Drainage Simulation Training
DOI: https://doi.org/10.21980/J8.52047Upon completing this lab session, the participant should have the capability to: 1) describe the indications, contraindications, and reasons for performing I&D of an abscess, 2) select the necessary equipment for performing I&D of an abscess, 3) demonstrate the necessary steps for performing
an I&D procedure on a simulated abscess.
Ultrasound Guided Peripheral Nerve Block Workshop: How to Take Your Residents from Zero to Hero
DOI: https://doi.org/10.21980/J8.52156After completing this small group workshop, the resident should be able to: 1) recognize the indications for the serratus anterior plane block, the posterior tibial block and the ulnar, median, and radial nerve blocks and the anatomical locations that would benefit from these blocks, 2) identify proper probe selection and placement, in addition to patient positioning, in order to perform these blocks, as well as anesthetic choice and dosing, 3) demonstrate knowledge of anatomical landmarks and areas to avoid evidenced by probe placement and positioning, 4) describe the steps to perform these nerve blocks, and 5) demonstrate knowledge of contraindications to these blocks as well as potential complications of these procedures and how to mitigate them.