Ophthalmology
A Multimodal Approach to Lateral Canthotomy and Cantholysis Training for Emergency Medicine Trainees: A Simulation Training Package
DOI: https://doi.org/10.5070/M5.52351By the end of this session, learners should be able to: 1) recognize the clinical features of OCS, 2) describe the indications and steps of performing LCC, 3) perform a lateral canthotomy and cantholysis procedure on a low-fidelity model, and 4) demonstrate improved confidence in recognizing and managing OCS.
A Case Report of Carotid Cavernous Fistula: A Commonly Missed Diagnosis
DOI: https://doi.org/10.5070/M5.52242The initial physical exam performed by the ED provider revealed severe left eye chemosis, clear drainage, visual acuity of right eye 20/100 and left eye 20/400, and a left eye IOP of 52. There was a deficit of extraocular movement in all directions of gaze and limitation in all visual fields in the left eye. The MRI showed that at the level of the eye, the left cavernous sinus is asymmetrically enlarged compared to the right (red arrow) with an enlarged left inferior petrosal sinus with internal flow void on the pre-contrast MRI images (blue arrow). The orange arrow notes a central filling defect of the left superior ophthalmic vein on the MRA.
A Case Report of Inferior Rectus Abscess
DOI: https://doi.org/10.21980/J8J35GNon-contrast computed tomography (CT) imaging of the head in coronal, sagittal, and axial planes revealed a distinct 1.7 x 2.2 x 1.4 cm peripherally enhancing fluid collection within the left inferior orbit, involving the inferior rectus (yellow circle). This lesion resulted in restricted extraocular motility due to structural compression of the left globe. Laboratory results showed a mildly elevated white blood cell count of 11.5/mm3 and otherwise normal results including C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
A Case of Painful Visual Loss – Managing Orbital Compartment Syndrome in the Emergency Department
DOI: https://doi.org/10.21980/J8N35DBy the end of this simulation, learners will be able to: 1) demonstrate the major components and a systematic approach to the emergency ophthalmologic examination, 2) develop a differential diagnosis of sight-threatening etiologies that could cause eye pain or vision loss, 3) demonstrate proficiency in performing potentially vision-saving procedures within the scope of EM practice.
The Clue is in the Eyes. A Case Report of Internuclear Ophthalmoplegia
DOI: https://doi.org/10.21980/J8DP9MThere was no appreciable esotropia or exotropia noted on straight gaze (yellow arrows). On extraocular muscle examination, patient was noted to have a complete left medial rectus palsy consistent with a left internuclear ophthalmoplegia (red arrow). This was evidence by both eyes easily gazing left (green arrows); however, with rightward gaze, her left eye failed to gaze past midline (red arrow).
Sonographic Retrobulbar Spot Sign in Diagnosis of Central Retinal Artery Occlusion: A Case Report
DOI: https://doi.org/10.21980/J8735PThe bedside ocular ultrasound (B-scan) was significant for small, hyperechoic signal (white arrow) in the distal aspect of the optic nerve, concerning for embolus in the central retinal artery. Subsequent direct fundoscopic exam was significant for a pale macula with cherry red spot (black arrow), consistent with central retinal artery occlusion (CRAO).
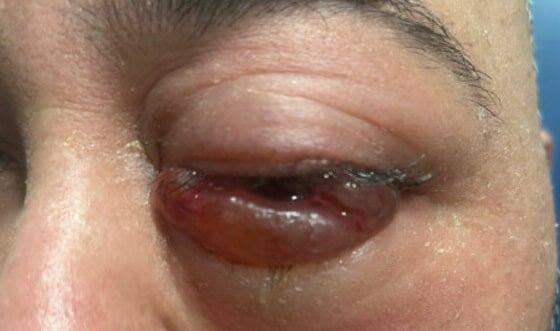
A Case Report of Invasive Mucormycosis in a COVID-19 Positive and Newly-Diagnosed Diabetic Patient
DOI: https://doi.org/10.21980/J81M1GOn physical exam, when the patient was asked to try and look to her right, the right eye failed to move laterally/abduct (blue arrow). Additionally, when asked to look straight ahead, the eye was slightly adducted (red arrow). There was a lack of motion of the right eye in abduction when the patient was asked to look to her right (yellow arrow).