Point-of-care Ultrasound in the Diagnosis and Monitoring of Bladder Hematoma vs. Hemorrhage
History of present illness:
A 55 year-old-male with benign prostatic hyperplasia (BPH) presented to the emergency department (ED) with oliguria, hematuria, and suprapubic abdominal pain for two days. The patient had undergone post-transurethral resection of prostate (TURP) two weeks prior and had his Foley catheter removed two days prior to presentation. His vital signs were unremarkable except for mild tachycardia. On examination, the patient had suprapubic tenderness and blood at the urethral meatus. Point-of-care ultrasound (POCUS) demonstrated 500mL of fluid in the bladder, half of which appeared hyperechoic and concerning for blood. Serial labs demonstrated a down-trending hemoglobin concerning for hematoma versus acute hemorrhage. Urinalysis was positive for greater than 182 red blood cells per high power field.
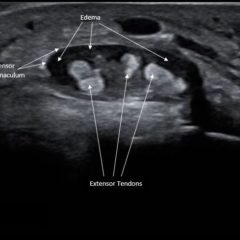
Significant findings:
Bladder POCUS demonstrated 500mL of post void residual fluid, indicative of retention. Half of the volume is hyperechoic (red circle); this is likely the bladder wall hematoma. Could also consider sonographic artifact, bladder mass, or cystitis.1-2
Discussion:
With a growing geriatric population, urinary retention secondary to BPH is becoming an increasingly common chief complaint. For individuals failing medical therapy, the TURP procedure is the gold standard for preventing urinary retention.3However, this procedure is not without complications, including postoperative hemorrhage and clot retention.4While the incidence of post-TURP hemorrhage has decreased recently, it remains a transfusion- requiring complication in up to 7% of patients.5
Postoperative bleeding after a TURP procedure is defined as occurring within one month of operation and is treated with continuous bladder irrigation (CBI) using a three-way Foley and clot extraction.6 Failure of the hematuria to resolve to light pink or clear urine warrants urologic consultation because the patient may require selective arterial prostatic embolization or packing of the prostatic cavity.5,7 Labs and vitals should be monitored with low threshold to administer intravenous fluids at first sign of hemodynamic compromise, such as tachycardia or hypotension. 8A urinalysis and culture should also be sent, as concomitant urinary tract infection is common.6
In this case, urology was consulted after CBI failed to clear the blood in the emergency department. The hematoma was flushed on the second attempt by the urologist using a three-way catheter. A foley was placed and the patient was discharged for outpatient follow up.
In summary, patients presenting with hematuria after recent urethral instrumentation should undergo bladder irrigation with close monitoring. There should be a low threshold for urologic consultation especially in the context of anemia, hemodynamic instability, or obstruction secondary to clots in order to reduce the morbidity and mortality of these patients.9 While the gold standard for diagnosing bladder injury as a cause of hematoma remains cystography (sensitivity and specificity of 95% and 100% respectively), ultrasound is a valuable tool in the emergency department for visualization of the bladder.10 Because current data regarding the efficacy of POCUS versus formal US in the diagnosis of bladder injury as the cause of hematuria is lacking, future studies are warranted.
Topics:
Bladder hematoma, hemorrhage, point of care ultrasound.
References/Suggestions for Further Reading:
- Cheng S, Phelkps A. Correlating the sonographic finding of echogenic debris in the bladder lumen with urinalysis. J Ultrasound Med. 2016; 35:1533-1540. doi:10.7863/ultra.15.09024.
- Hertzberg BS, Bowie JD, King LR, Webster GD. Augmentation and replacement of cystoplasty: sonographic findings. Radiology. 1987; 165:853-856. doi: 10.1148/radiology.165.3.3317511.
- Izard J, Nickel JC. Impact of medical therapy on transurethral resection of the prostate: two decades of change. BJU Int. 2011;108(1):89-93. doi: 10.1111/j.1464-410X.2010.09737.x.
- Teo S, Lee YM, Ho HS. An update on transurethral surgery for benign prostatic obstruction. Asian J Urol. 2017;4(3):195-198. doi: 10.1016/j.ajur.2017.06.006.
- Lynch M, Sriprasad S, Subramonian K, Thompson P. Postoperative haemorrhage following transurethral resection of the prostate (TURP) and photoselective vaporization of the prostate (PVP). Ann R Coll Surg Engl. 1997: 80(1):111-115. doi: 10.1308/003588410X12699663903557a.
- Cornu JN, Herrmann T, Traxer O, Matlaga B. Prevention and management following complications from endourology procedures. Eur Urol Focus. 2016:2(1):49-59. doi: 10.1016/j.euf.2016.03.014.
- Tan L, Venkatesh SK, Consigliere D, Heng CT. Treatment of a patient with post-TURP hemorrhage using bilateral SAPE. Nat Rev Urol. 2009; 6(12):680-685. doi: 10.1038/nrurol.2009.215.
- Hicks D, Li CY. Management of macroscopic hematuria in the emergency department. Emerg Med J. 2007;24(6): 385-390. doi; 10.1136/emj.2006.042457.
- Topaktas R, Altin S, Aydin C, et al. Retrospective evaluation of urological admissions to emergency service of a training and research hospital. Turk J Urol. 2014;40(4):216-220. doi: 10.5152/tud.2014.77861.
- Quagliano PV, Delair SM, Malhotra AK. Diagnosis of blunt bladder injury: A prospective comparative study of computed tomography cystography and conventional retrograde cystography. J Trauma. 2006;61(2):410. doi: 10.1097/01.ta/0000229940.36556.bf.