Point-Of-Care Ultrasound for the Diagnosis of Extensor Tenosynovitis
History of present illness:
A 21-year-old male presented to the emergency department (ED) with left-hand pain after hitting the dorsal aspect of the hand on a piece of metal while riding a bike the day prior. The physical exam was notable for swelling of the dorsal aspect of the left hand with erythema, diffuse dorsal wrist tenderness to palpation, and limited active range of motion in all anatomical planes secondary to pain of the wrist. There was a small 0.5cm scabbed over puncture lesion on the dorsal aspect of the hand. There was no drainage, fluctuance, or loss of sensation. Laboratory work showed leukocytosis. Point-of-care ultrasound (POCUS) was performed to assess for pathology.
Significant findings:
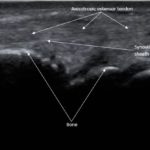
Point-of-care ultrasound of the dorsal aspect of the left hand reveals a heterogenous hypoechoic fluid collection surrounding the extensor tendons (axial view) within the retinaculum consistent with edema. Longitudinal view shows anechoic fluid within the tenosynovium which is located between the anisotropic extensor tendon and linear hyperechoic synovial sheath. Longitudinal view also shows some cobblestoning, or tissue edema, superficial to the anisotropic extensor tendon. The patient’s contralateral right dorsal hand was scanned in a longitudinal view and shows no cobblestoning or hypoechoic fluid under the synovial sheath. The patient was diagnosed with tenosynovitis, and started on intravenous antibiotics.
Discussion:
Tenosynovitis is the inflammation or infection of a tendon and its synovial sheath, which can occur in any joint, though it is most frequently seen in the hands and wrist.1 Within the wrist, infectious tenosynovitis is more commonly described in the flexor tendons, and less commonly in the extensor tendons.2 Etiologies of infectious tenosynovitis include trauma with direct inoculation, hematogenous spread, and contiguous spread from adjacent tissues.1 The most common pathogens due to trauma are the gram-positive skin flora such as Staphylococcus aureusand Streptococcus.3 Treatment of flexor tenosynovitis always includes adequate surgical drainage with empiric antibiotics due to the limited anatomic space with possible early tendon necrosis.2 Contrarily, extensor tenosynovitis can be treated with observation with intravenous antibiotic coverage since the extensor tendons lack a retinacular system and infections tend to be less loculated.2
There is a paucity of literature on extensor tenosynovitis compared with flexor tenosynovitis. The diagnosis of tenosynovitis of the wrist is often clinical using Kanavel’s cardinal signs developed in 1912, though this was developed for flexor, and not extensor tenosynovitis.1 More recently, ultrasound has been used to diagnose tenosynovitis with a sensitivity of 94% and has been shown to be more sensitive than clinical exam.4,5,6 Ultrasound findings may include hypoechoic to anechoic fluid and cobblestoning of the soft tissues, a thickened tendon sheath, and abnormal hypoechoic material within the synovial sheath.5 These ultrasound findings are best seen using a high frequency linear probe oriented in the transverse and longitudinal planes over the dorsal aspect of the hand.6 Our patient’s ultrasound demonstrated cobblestoning of the soft tissues and abnormal hypoechoic material within the synovial sheath; however, we did not measure synovial sheath thickness. While superficial cobblestoning is commonly seen in cellulitis, a thickened synovial sheath and/or abnormal hypoechoic material within the synovial sheath should prompt consideration of tenosynovitis.
Our patient was started on intravenous clindamycin and ceftriaxone in the ED. He was admitted for observation. X-ray of the hand did not reveal any osteomyelitis. On the following day, the patient’s edema and erythema significantly decreased and his leukocytosis resolved. He was subsequently discharged with prescriptions for oral clindamycin and cephalexin with instructions to follow-up with his primary care provider as an outpatient. Three weeks later, the patient was noted to have complete resolution of his symptoms.
Topics:
Ultrasound, point of care ultrasound, tenosynovitis, soft tissue, wrist.
References:
- Padrez K, Bress J, Johnson B, Nagdev A. Bedside ultrasound identification of infectious flexor tenosynovitis in the emergency department. West J Emerg Med. 2015;16(2):260-262. doi: 10.5811/westjem.2015.1.24474
- Newman ED, Harrington TM, Torretti D, Bush DC. Suppurative extensor tenosynovitis caused by Staphylococcus aureus. J Hand Surg Am. 1989;14(5):849-851.
- Small LN, Ross JJ. Suppurative tenosynovitis and septic bursitis. Infect Dis Clin North Am. 2005;19(4):991-1005, xi. doi: 10.1016/j.idc.2005.08.002
- Hmamouchi I, Bahiri R, Srifi N, Aktaou S, Abouqal R, Hajjaj-Hassouni N. A comparison of ultrasound and clinical examination in the detection of flexor tenosynovitis in early arthritis. BMC Musculoskelet Disord. 2011;12:91. doi: 10.1186/1471-2474-12-91
- Jardin E, Delord M, Aubry S, Loisel F, Obert L. Usefulness of ultrasound for the diagnosis of pyogenic flexor tenosynovitis: A prospective single-center study of 57 cases. J Hand Surg Am. 2018;37(2):95-98. doi: 10.1016/j.hansur.2017.12.004
- Alcalde M, D’Agostino MA, Bruyn GA, et al. A systematic literature review of US definitions, scoring systems and validity according to the OMERACT filter for tendon lesion in RA and other inflammatory joint diseases. Rheumatology (Oxford). 2012;51(7):1246-1260. doi: 10.1093/rheumatology/kes018