A Toddler with Abdominal Pain and Emesis
History of present illness:
A 3-year-old male presented to the emergency department (ED) with three days of progressively worsening diffuse abdominal pain. He also had associated nausea, vomiting, decreased oral intake, and subjective fevers. He was found to be in moderate distress with tachycardia, diffuse abdominal tenderness, guarding, and refusal to jump up and down. In the ED, he was afebrile and had no leukocytosis. Bedside ultrasound of the right lower quadrant of the abdomen showed findings consistent with acute appendicitis, which was confirmed with a formal ultrasound. The patient was given ceftriaxone and metronidazole, and transferred to a children’s hospital for appendectomy.
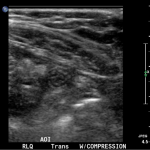
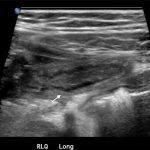
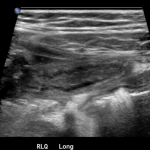
Significant findings:
In the long axis video, the appendix appears as an enlarged, non-compressible, blind-ending tubular structure (white arrow) with distinct appendiceal wall layers and lack of peristalsis. In the short axis video, the appendix appears as a target sign (yellow arrow) between the abdominal and psoas muscles. The maximal outer diameter (MOD) measures 11.8mm and the appendix wall measures 0.17mm. There is trace adjacent free fluid and echogenic periappendiceal fat. Transverse axis video and image (red arrow) demonstrate that the appendix is not compressible. These findings are consistent with acute appendicitis.
Discussion:
Acute appendicitis is the most common surgical emergency in the pediatric population, with an annual incidence of 119.7 cases/100,000 in children of age 0-19 years.1,2 Given children’s limited ability to communicate their symptoms and the radiation risks associated with computed tomography, ultrasound is a particularly valuable tool for diagnosing appendicitis in children. It has a sensitivity and specificity of 88% and 94%, respectively, compared to the 94% sensitivity and 95% specificity seen for CT studies.3,4 Frequent use of ultrasound and clear visualization of the appendix during exam improve sensitivity.2 Currently, the diagnostic criteria for appendicitis includes a MOD of compressed appendix >6mm (most specific sign) and an appendix wall thickness ≥3 mm.4,5 A retrospective review at one institution found that the highest sensitivity (98.7%) and specificity (95.4%) were achieved when MOD was ≥7 mm or wall thickness was >1.7 mm.5 Male gender, increased age, and body mass index percentiles ≥85 are associated with non-diagnostic ultrasound.6,7 Use of lower frequency curvilinear transducer for retrocecal appendices and obese children and techniques such as posterior manual compression, where the operator’s left hand provides anterior force to the patient’s right lower back above the ileum to reduce the distance to the transducer, may be helpful.4
Topics:
Acute appendicitis, ultrasound, abdominal pain, emesis.
References:
- Anderson JE, Bickler SW, Chang DC, Talamini MA. Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995-2009. World J Surg. 2012;36(12):2787-94. doi: 10.1007/s00268-012-1749-z
- Mittal MK, Dayan PS, Macias CG, Bachur RG, Bennett J, Dudley NC, et al. Performance of ultrasound in the diagnosis of appendicitis in children in a multicenter cohort. Acad Emerg Med. 2013;20(7):697-702. doi: 10.1111/acem.12161
- Doria AS, Moineddin R, Kellenberger CJ, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006;241(1):83-94. doi: 10.1148/radiol.2411050913
- Reddan T, Corness J, Mengersen K, Harden F. Ultrasound of paediatric appendicitis and its secondary sonographic signs: providing a more meaningful finding. J Med Radiat Sci. 2016;63(1):59-66. doi: 10.1002/jmrs.154
- Goldin AB, Khanna P, Thapa M, McBroom JA, Garrison MM, Parisi MT. Revised ultrasound criteria for appendicitis in children improve diagnostic accuracy. Pediatr Radiol. 2011;41(8):993-999. doi: 10.1007/s00247-011-2018-2
- Keller C, Wang NE, Imler DL, Vasanawala SS, Bruzoni M, Quinn JV. Predictors of nondiagnostic ultrasound for appendicitis. J Emerg Med. 2016;S0736-4679(16)30557-1. doi: 10.1016/j.jemermed.2016.07.101
- Schuh S, Man C, Cheng A, Murphy A, Mohanta A, Moineddin R, et al. Predictors of non-diagnostic ultrasound scanning in children with suspected appendicitis. J Pediatr. 2011;158(1):112-118. doi: 10.1016/j.jpeds.2010.07.035