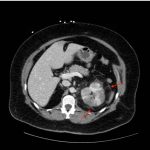
Acute Pyelonephritis with Perinephric Stranding on CT
History of present illness:
A 54-year old female presented to the emergency department with complaints of fevers, dysuria, urinary frequency, and diffuse abdominal pain. Her temperature was 103°F, but the remainder of her vital signs were normal. Upon physical examination, the patient had tenderness to palpation in the left upper and left lower abdomen and left costovertebral angle tenderness. Due to the location of pain (diverticulitis is in the differential for left-sided abdominal pain in this age group) and patient’s reported history of nephrolithiasis, a computed tomography (CT) scan of the abdomen and pelvis with intravenous (IV) contrast was ordered because the physician felt this could best work up both of these possible conditions.
Significant findings:
A CT abdomen and pelvis with IV contrast showed neither nephrolithiasis nor diverticulitis, and instead showed heterogeneous enhancement of the left kidney with mild edematous enlargement and striated left nephrogram. Significant perinephric stranding (red arrows) was also noted and was consistent with severe acute pyelonephritis.
Discussion:
Acute pyelonephritis (APN) is a bacterial infection of the renal parenchyma which can present with a spectrum of symptoms including flank pain, high-grade fever, vomiting, and urinary tract symptoms.1,2 The diagnosis of APN can be made based on these clinical features with associated laboratory findings of bacteriuria, pyuria, positive urine cultures, and leukocytosis.1,2,7 Early diagnosis and treatment of APN is essential to prevent complications such as renal abscess or infarct, which could lead to renal failure, sepsis, and shock.3
Computed tomography has a sensitivity and specificity of 86.8% and 87.5%, respectively, for diagnosing APN. Common findings include striated nephrograms or perinephric fat stranding.2 However, imaging is not required for diagnosis and is typically reserved for patients who are immunocompromised, have severe symptoms, or show no clinical improvement 72 hours after initiating antibiotic therapy.2,3,4 The diagnosis acute pyelonephritis is mostly done using clinical judgment. A patient’s history, physical exam, and confirmatory labs including urinalysis is usually sufficient for the diagnosis. Proper diagnosis and treatment of APN has been of increasing concern in community settings due to increasing rates of antimicrobial resistance in uropathogens.5,6,7 Therefore, monitoring of local antibiotic resistance trends through urine cultures is essential for proper management of these patients in the emergency department.7
Topics:
Acute pyelonephritis, perinephric stranding, nephrogram.
References:
- Isreal RS, Lowenstein SR, Marx JA, Koziol-McLain J, Svoboda L, Ranniger S. Management of acute pyelonephritis in an emergency department observation unit. Ann Emerg Med. 1991;20(3):253-7.
- Stunnell H, Buckley O, Feeney J, Geoghegan T, Browne RF, Torreggiani WC. Imaging of acute pyelonephritis in the adult. EurRadiol. 2007;17(7):1920-1928. doi: 10.1007/s00330-006-0366-3
- Chen KC, Hung SW, Seow VK, Chong CF, Wang TL, Li YC, et al. The role of emergency ultrasound for evaluating acute pyelonephritis in the ED. Am J Emerg Med. 2011;29(7):721-724. doi: 10.1016/j.ajem.2010.01.047
- Goel RH, Unnikrishnan R, Remer EM. Acute urinary tract disorders.Radiol Clin North Am. 2015;53(6):1273-1292. doi: 10.1016/j.rcl.2015.06.011
- Doi Y, Park YS, Rivera JI, Adams-Haduch JM, Hingwe A, Sordillo EM, et al. Community-associated extended-spectrum beta-lactamase–producing Escherichia coli infection in the United States. Clin Infect Dis.2013;56(5):641-648. doi: 10.1093/cid/cis942
- Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med.2012;366(11):1028-1037. doi: 10.1056/NEJMcp1104429
- Park YS, Oh WS, Kim Y, Yeom JS, Choi HK, Kwak YG, et al. Health-care associated acute pyelonephritis is associated with inappropriate empiric antibiotic therapy in the ED. Am J Emerg Med. 2016;34(8):1415-20. doi: 10.1016/j.ajem.2016.04.018