Wandering Spleen
History of present illness:
A 7-month-old boy presented for evaluation of an abdominal mass. Two weeks prior, the patient had a fever followed by 24 hours of vomiting and abdominal pain, which self-resolved. His pediatrician noted the mass on exam and referred child to the emergency department (ED). His abdominal exam was significant for a hard mass palpated to the left of the umbilicus.
Significant findings:
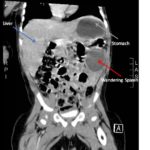
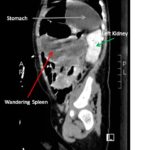
Computed tomography (CT) of the abdomen showed displacement of spleen (red arrow), lying in the left mid abdomen anterior to the left kidney (green arrow), and inferior to the stomach (grey arrow). The spleen is normally located in the left upper quadrant of abdomen just inferior to the diaphragm. The liver (blue arrow) is in the proper anatomic position in the right upper quadrant and of normal density. The spleen is diffusely hypodense, with a visible capsule representing an enlarged, wandering spleen with complete infarction without evidence of free fluid or rupture.
A normal spleen should have a density appearance similar to that of the liver, due to the intravenous contrast and should appear white on CT imaging in the vasculature and body of the organ. The splenic capsule often has a separate blood supply compared to the splenic body, thus is also white on the imaging, and despite the infarction of the spleen, is seen highlighting the outline of the organ.
Discussion:
A wandering spleen is a rare condition with a reported incidence of < 0.2% of birth defects.1 Most commonly, it is diagnosed in patients under one year of age with a male predominance of 6:1.2 The pathophysiology is a loss or weakening of the ligaments that hold the spleen fixed causing the spleen to “wander” from its normal anatomic position. Most cases are thought to be congenital, but there are cases of acquired wandering spleen secondary to abdominal trauma. One third of all reported cases are in children. In a majority of cases, a wandering spleen is asymptomatic. Patients can also present with splenomegaly, an unspecified abdominal mass, recurrent episodes of abdominal pain, intestinal obstruction, nausea, vomiting, or fever. It is thought that the abdominal pain typically comes in episodes when the splenic vasculature is twisting and untwisting due to its mobility.3
In the emergency department, prompt and thorough evaluation of the abdomen is critical to rule out an acute surgical abdomen. Patients with a wandering spleen can present with acute hemorrhage, as well as ischemia. Monitoring complete blood counts, pain control, and appropriate fluid resuscitation are necessary.
Treatment of a wandering spleen is a splenopexy to surgically fixate the spleen in the left upper quadrant. However, if there is no blood flow to the spleen even after detorsing, a splenectomy is performed.4 At the time of our patient’s presentation, the spleen was completely infarcted with evidence of ischemia on CT scan. The likelihood of return flow to the spleen was deemed unlikely. The decision was made to delay surgery because the spleen will likely necrose and surgery can be performed electively on an outpatient basis if required. Some recommendations for similar cases state that splenectomy is necessary in cases of completely infarcted spleens, especially if the presentation is an acute surgical abdomen.2,3 The decision to not operate at the time of presentation is indicative of the most conservative management of a wandering spleen.2,3 Ifthe patient suffers complications with conservative management, such as chronic abdominal pain, abnormal enlargement of the spleen, and/or abnormalities of the complete blood count, the treatment of choice is to proceed with splenectomy.3
As a result of the wandering spleen, patients become functionally asplenic, and are at risk for invasive bacterial infections from encapsulated organisms. Thus, especially for younger patients, prophylactic antibiotics are indicated; our patient was started on prophylactic penicillin at time of discharge from the ED.
Topics:
Wandering spleen, pediatric abdominal masses.
References:
- Turhan A, Kapan S, Gonenc M, Dogan M, Aygun E. Wandering spleen: report of two cases. Int Med Case Rep J. 2010;3(1):19-22. doi: 10.2147/IMCRJ.S8937.
- Allen K, Andrews G. Pediatric wandering spleen—the case for splenopexy: review of 35 reported cases in the literature. J Pediatr Surg. 1989;24(5):432-435. doi: 10.1016/S00223468(89)80395-1.
- National Organization for Rare Disorders. Wandering spleen. https://rarediseases.org/rare-diseases/wandering-spleen/. Published 2008. Accessed June 2, 2018.
- Alqadi GO, Saxena AK. Is laparoscopic approach for wandering spleen in children an option? J Minim Access Surg. 2018. doi: 10.4103/jmas.JMAS_14_18.