Spontaneous Intracranial Hemorrhage in Severe Hemophilia A: A Rare Cause of Seizure in a Young Child
History of present illness:
A 5-month-old male born full-term presented with fever to 102.3°F and an episode of left arm stiffening and shaking with blinking. The episode lasted 45 minutes after which it spontaneously resolved. Review of symptoms was negative for poor feeding, vomiting or trauma. His medical history was negative for bleeding disorders, easy bruising, or seizures. Family history was noncontributory. Vital signs were normal. He had a witnessed 3-minute focal seizure with rhythmic jerking of his left arm and lip-smacking during the examination. He lacked clonus or cranial nerve anomalies; his tone and deep tendon reflexes were normal. He had no cutaneous stigmata. He had no bruising, swelling, or tenderness to palpation over his head or body.
Significant findings:
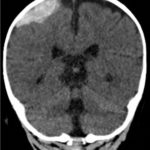
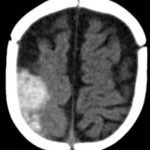
A computed tomography (CT) scan of the head without contrast was obtained out of concern for intracranial pathology due to the patient’s young age and the witnessed focal seizure. The CT showed a 4.2 x 1.2 x 1.5 cm acute extra-axial intracranial right frontoparietal hemorrhage favoring epidural over subdural hemorrhage given its lenticular shape. There was no underlying fracture, herniation or midline shift identified.
Given the concern for non-accidental trauma in this nonmobile child with no history of trauma, pediatric surgery and neurosurgery were consulted and further bloodwork was obtained, revealing elevated partial thromboplastin time (PTT) and a normal prothrombin time (PT). Further work-up led to a diagnosis of severe hemophilia A. He was managed non-operatively with factor VIII infusions to achieve normal factor levels. He remained neurologically stable without further seizure activity during his hospitalization. A skeletal survey showed no fractures. He received levetiracetam for 6 months and had no neurological deficits.
Discussion:
Hemophilia is a rare inherited bleeding disorder caused by a deficiency of factor VIII (hemophilia A) or factor IX (hemophilia B). It affects an estimated 0.01% of the population.1 It is characterized as mild, moderate, or severe, based on factor levels, which typically correlate with the degree of bleeding symptoms.
Spontaneous intracranial hemorrhage (ICH) is a rare complication of hemophilia, with a frequency of 2.2%-7.8% and a mortality of 34%.2,3 It is a life-threatening complication that requires emergent management depending on the size and severity of the bleeding. Larger hemorrhages with mass effect and midline shift may require neurosurgical intervention whereas smaller hemorrhages may be managed conservatively with factor infusions.
In the absence of known trauma in a nonmobile child, ICH is highly concerning for child abuse. In this setting, it is vital to screen for other injuries and comorbid conditions. No studies have systematically compared the presentation, clinical findings, patterns of ICH, or presence of retinal hemorrhages found in children with bleeding disorders with those found in children in whom abusive head trauma is diagnosed.4 However, bleeding disorders can cause ICH in any part of the cranial contents, and up to 12% of children and young adults with bleeding disorders have had ICH at some point in time.4 In severe bleeding episodes that are potentially life-threatening such as ICH, treatment with factor should be initiated immediately, even before the diagnostic assessment, such as CT imaging, is complete. Since factor levels may not be immediately available, an initial dose of 50 units/kg of factor VIII should be given for hemophilia A or 100-120 units/kg of factor IX for hemophilia B.1 These doses assume negligible baseline factor levels. Early consultation with hematology is essential. Children with long-standing hemophilia may have inhibitors, necessitating use of different medications.
Topics:
Intracranial hemorrhage (ICH), bleeding disorders, hemophilia, seizure.
References:
- Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. Guidelines for the management of hemophilia. Haemophilia. 2013;19(1): e1-47. doi: 10.1111/j.1365-2516.2012.02909.x.
- Hegde A, Nair R, Upadhyaya S. Spontaneous intracerebral hemorrhage in hemophiliacs—A treatment dilemma. Int J Surg Case Rep. 2016;29:17-19. doi: 1016/j.ijscr.2016.10.046.
- Martinowitz U, Heim M, Tadmor R, et al. Intracranial hemorrhage in patients with hemophilia. Neurosurgery. 1986;18(5):538–541. doi: 10.1227/00006123-198605000-00004.
- Anderst JD, Carpenter SL, Abshire TC. Evaluation for bleeding disorders in suspected child abuse. Pediatrics. 2013;131(4):e1314-1322. doi: 10.1542/peds.2013-0195.