Search By Keyword
Found 645 Unique Results
Page 4 of 65
Page 4 of 65
Page 4 of 65
Drowning Complicated by Hypothermia
DOI: https://doi.org/10.21980/J8QS7PAt the conclusion of the simulation session, learners will be able to: 1) obtain a relevant focused history, including circumstances of drowning and/or cold exposure; 2) outline different clinical presentations of hypothermia, loosely correlated with core temperature readings; 3) discuss management of hypothermia, including passive external rewarming, active external rewarming, active internal rewarming, and extracorporeal blood rewarming; 4) discuss pathophysiology of drowning; 5) identify appropriate disposition of patients who present after drowning; and 6) identify appropriate disposition of hypothermic patients.
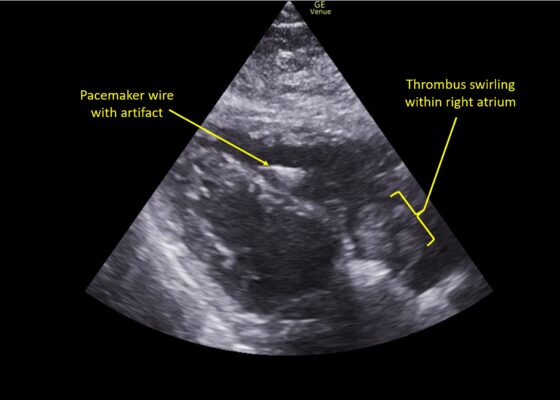
A Case Report of Right Atrial Thrombosis Complicated by Multiple Pulmonary Emboli: POCUS For the Win!
DOI: https://doi.org/10.21980/J8TM07Pulmonary POCUS was performed by the ED physician (GE Venue, C1-5-RS 5MHz curvilinear transducer), and lung examination was unremarkable with no pleural effusion, pneumothorax, or infiltrate. Subxiphoid views (GE Venue, 3Sc-RS 4MHz phased-array transducer) were obtained because this patient’s COPD with severe pulmonary hyperexpansion made parasternal and apical 4-chamber views suboptimal. A large thrombus can be seen within the right atrium (movie 1, images 1, 2). This has a serpiginous, rounded appearance and is mobile, appearing to swirl within the right atrium with intermittent extrusion through the tricuspid valve. A pacemaker wire is also visible within the right ventricle as a non-moving, hyperechoic, linear structure with posterior enhancement artifact. Pericardial effusion is not present.
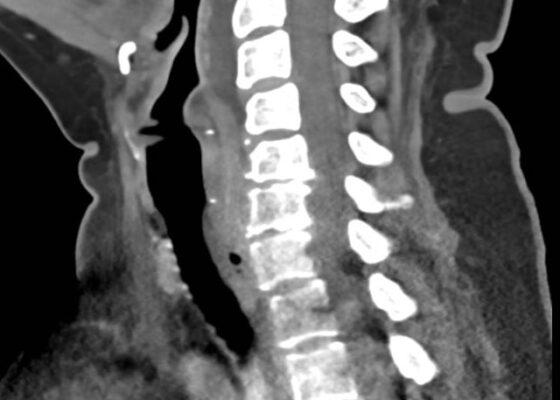
Retropharyngeal Abscess in an Adult Patient Presenting with Neck Fullness and Dysphagia: A Case Report
DOI: https://doi.org/10.21980/J8M36GContrast-enhanced CT soft tissue of the neck showed evidence of a prevertebral/retropharyngeal fluid collection, extending from the odontoid tip to the inferior C4 vertebral body margin, measuring 5.4 x 1.0 x 3.3 centimeters (cm) in size (yellow lines) without gross airway narrowing.
The Advantage of Using Video Laryngoscope in Puncture and Incisional Drainage of Peritonsillar Abscess: A Case Report
DOI: https://doi.org/10.21980/J8G935Incision of the peritonsillar abscess was performed with the assistance of the C-MAC video laryngoscope which provided a clear, illuminated, and unobstructed view of the incision site. Local anesthesia with 1% xylocaine was administered, and the abscess was incised with a scalpel and drained with a forceps.
A Case Report on an Elusive Incident of Erythema Multiforme
DOI: https://doi.org/10.21980/J8BM0WHer physical exam was notable for multiple scattered tense vesicles on an erythematous base along the left and right lower extremities and right upper extremity. The lesions were excoriated and in different stages of evolution. No oral, mucosal, or conjunctival lesions were found. Physical exam was otherwise unremarkable.
A Case of Painful Visual Loss – Managing Orbital Compartment Syndrome in the Emergency Department
DOI: https://doi.org/10.21980/J8N35DBy the end of this simulation, learners will be able to: 1) demonstrate the major components and a systematic approach to the emergency ophthalmologic examination, 2) develop a differential diagnosis of sight-threatening etiologies that could cause eye pain or vision loss, 3) demonstrate proficiency in performing potentially vision-saving procedures within the scope of EM practice.
Going in Blind: A Common Scenario in an Uncommon Situation
DOI: https://doi.org/10.21980/J8RS8CBy the end of this simulation, learners will be able to (1) evaluate and treat a patient experiencing myocardial infarction and subsequent cardiac arrest during a power outage, (2) describe the local protocols for managing patient care during a power outage, (3) demonstrate the ability to coordinate a medical team during a simulated power outage in an emergency department with limited resources, (4) manage a cardiac arrest patient by following Advanced Cardiac Life Support (ACLS) protocols for bradycardia and ventricular fibrillation, and (5) justify the urgency of transfer to a certified ST segment elevation myocardial infarction center/cardiac intensive care unit, referencing the recommended 120-minute door-to-balloon time.
Actively Teaching Active Teaching Techniques
DOI: https://doi.org/10.21980/J8H94VBy the end of this small group exercise, learners will be able to: 1) assess interactive teaching techniques that support learning in various environments; 2) incorporate active teaching techniques into a variety of real-world teaching scenarios; 3) implement selected techniques to enrich one’s own teaching practice.
A Whodunit Gamified Flipped Classroom For High Yield Bite Injuries And Envenomation
DOI: https://doi.org/10.21980/J88S81By the end of this activity, learners will be able to: 1) identify and name species responsible for bite/sting/envenomation injuries, 2) recognize associated signs, symptoms, physical exam findings and complications associated with bites/stings/envenomations by certain species, 3) discuss management such as antibiotics, antivenom, and supportive care.
Bridging Hospital Resource Variability: Adapting the Escape Room to Integrate Procedure Teaching for Emergency Medicine Trainees in India
DOI: https://doi.org/10.21980/J8CK98By the end of the escape room, learners should be able to: 1) describe the mechanism of action of antiretroviral therapies available in India, 2) prescribe initial antiretroviral therapy to a patient presenting to the emergency department with a new diagnosis of HIV, 3) develop a differential diagnosis for a patient with HIV presenting to the ED with chest pain, 4) identify common dermatologic manifestations of opportunistic infections in patients with HIV, 5) identify computerized tomography scan and lumbar puncture features for central nervous system infections seen in patients with Acquired Immunodeficiency Syndrome (AIDS), 6) identify red flag features and appropriate workup for a patient with HIV presenting with a headache to the ED, 7) interpret images obtained during a Rapid Ultrasound for Shock and Hemorrhage (RUSH) exam, 8) identify cardiac tamponade and perform a pericardiocentesis, and 9) communicate and collaborate as a team to manage a complex, unstable patient with HIV in the ED.