The Role of Chest X-Ray and Bedside Ultrasound in Diagnosing Pulmonary Bleb versus Pneumothorax
History of present illness:
A 48-year-old male with chronic obstructive pulmonary disease (COPD) presented to the emergency department with stabbing chest pain to the right lower rib region along the axillary line. On examination, patient had no visible trauma, but was in mild respiratory distress with absent breath sounds on the right side. The patient’s oxygen saturation ranged in the 90s on room air during his encounter, but otherwise had unremarkable vital signs.
Significant findings:
The patient was evaluated with bedside ultrasound for concern of possible pneumothorax. Imaging of the left lung with M-mode demonstrated a “sea shore” sign showing a wavy pattern below the pleural line caused by lung sliding as well as “comet tail” artifact caused by from the deep pleura. However, there was no lung sliding on the right shown by a lack of “comet tail” artifact and a “bar code” sign where M-mode shows straight lines throughout the image, this is caused by lack of motion below the pleura. This lack of lung sliding is consistent with possible pneumothorax or bleb.
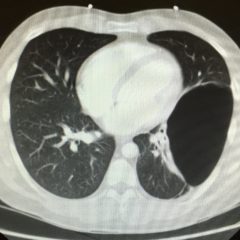
A two-view chest X-ray (CXR) revealed absent lung parenchyma in the right lung similar to a large pneumothorax (see red outline). Electronic medical record chart review revealed previous CXRs with similar findings. This patient was determined to have an acute COPD exacerbation with chronic blebs, but no pneumothorax.
Discussion:
Pulmonary blebs are collections of air in the alveolar layer of the pleura formed by a rupture of the alveolar wall.1 They can leak air into chest cavity leading to a high rate of recurrent spontaneous pneumothorax.2 Chest X-rays (CXR) are the current gold standard in diagnosing pneumothorax. A recent study among 192 critically ill patients showed CXR has high diagnostic accuracy and positive predictive value, at 90.6% and 95.0%, respectively.3 Visible visceral pleural lines on CXR seen without distal lung markings is usually diagnostic of pneumothorax.4 In this case however, the patient’s CXR and lung ultrasound findings were similar to standard pneumothorax findings, however chart review demonstrated the patient had a known large pulmonary bleb.
The treatment for pneumothorax is chest tube insertion. To avoid unnecessary chest tube placement, emergency physicians must consider pulmonary blebs as a diagnosis in patients with mild respiratory distress who have a large area of absent lung parenchyma and visible visceral pleural lines on CXR. If a clinician is unsure and does not have access to previous imaging, a computed tomography scan of the chest can be used to clarify the diagnosis.5
This patient was conservatively managed with oral prednisone, intravenous morphine sulfate, combination albuterol-ipratropium nebulizer treatment, and later discharged for pulmonology follow up.6 The patient did not require any further imaging during this visit. In recurrent disease or severe dyspnea, bullectomy may be indicated.
Topics:
Ultrasound, X-ray, pulmonary blebs, pneumothorax.
References:
- Massie JR, Welchons GA. Pulmonary Blebs and Bullae. Annals of Surgery. 1954;139(5):624-632.
- Casali C, Stefani A, Ligabue G, et al. Role of Blebs and Bullae Detected by High-Resolution Computed Tomography and Recurrent Spontaneous Pneumothorax. The Annals of Thoracic Surgery. 2013;95(1):249-255.
doi: 10.1016/j.athoracsur.2012.05.073 - Abdalla W, Elgendy M, Abdelaziz A, Ammar M. Lung ultrasound versus chest radiography for the diagnosis of pneumothorax in critically ill patients: a prospective, single-blind study. Saudi Journal of Anaesthesia. 2016;10(3):265-269. doi: 10.4103/1658-354X.174906
- O’Connor AR, Morgan WE. Radiological review of pneumothorax. BMJ: British Medical Journal. 2005;330(7506):1493-1497
- Mitlehner W, Friedrich M, Dissmann W. Value of computer tomography in the detection of bullae and blebs in patients with primary spontaneous pneumothorax. Respiration. 1992;59(4):221–227 doi:10.1159/000196062
- Rokicki W, Rokicki M, Wojtacha J, Filipowski M, Dżejlili A, Czyżewski D. Is it possible to standardize the treatment of primary spontaneous pneumothorax? Part 1: etiology, symptoms, diagnostics, minimally invasive treatment.Kardiochir Torakochirurgia 2016;13(4):322-327. doi:10.5114/kitp.2016.64874