Pneumocystis jirovecii (carinii) Pneumonia
History of present illness:
A 62-year-old male with a past medical history of untreated human immunodeficiency virus (HIV) presented to the emergency department with one month of shortness of breath, non-productive cough, and fevers. He had been seen by an outpatient provider and was given amoxicillin, though his symptoms did not improve.
His vital signs included a temperature of 102°F, heart rate of 108 beats/min, BP 90/60 mm Hg, and an oxygen saturation of 60% on room air. He was placed on 15L non-rebreather mask with improvement in saturation to 97%. His exam showed tachypnea with normal breath sounds.
Labs showed a white blood cell count of 8.4 x 1000/mm3without bands, complete metabolic panel remarkable only for a total bilirubin of 3.0, and a lactic acid dehydrogenase (LDH) of 444. Lactate was normal.
Significant findings:
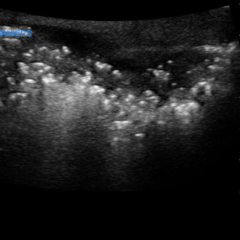
Chest X-ray showed diffuse, patchy interstitial and alveolar infiltrates bilaterally concerning for Pneumocystis jirovecii(previously Pneumocystis carinii) pneumonia (PJP). The AP radiograph (top left figure) showed the classic “bat-wing” distribution on the left side. Repeat radiograph (bottom figure) one day after admission showed worsening of the infiltrates.
Discussion:
Pneumocystis jiroveciipneumonia is most common in HIV patients with CD4 counts less than 200. Physical exam findings include crackles and rhonchi; however, 50% of presentations include benign pulmonary exams.1 On chest radiograph, the most common findings are diffuse bilateral interstitial infiltrates. In one study, 25% of radiographs showed alveolar or mixed interstitial-alveolar patterns, and 10% of radiographs included localized infiltrates, hilar enlargement, cysts, or honeycombing.2 In other studies of patients with mild to moderate PJP, 39% of radiographs were normal.3 After diagnosis is made or if suspicion for PJP is high, standard treatment is sulfamethoxazole/trimethoprim (TMP-SMX)15-20 mg/kg/day TID or QID. Prednisone 40 mg BID is added to the TMP-SMX if the patient’s A-a gradient is higher than 35, or if the PO2 is less than 70 mmHg on room air.4,5 After finishing treatment, prophylactic TMP-SMX should be given to all patients with CD4 counts less than 200 to prevent future recurrence until their CD4 counts recover on highly active antiretroviral therapy.
This patient was admitted to the intensive care unit for hypoxic respiratory distress and pneumonia. He was started on vancomycin and cefepime; TMP-SMX and corticosteroids were added for presumed PJP. Diagnosis was later confirmed and the patient eventually made a full recovery.
Topics:
Respiratory, PCP pneumonia, pneumocystis jirovecii (carinii).
References:
- Kales CP, Murren JR, Torres RA, Crocco JA. Early predictors of in-hospital mortality for Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome. Arch Intern Med. 1987;147(8):1413-1417. doi: 1001/archinte.1987.00370080049012
- DeLorenzo LJ, Huang CT, Maguire GP, Stone DJ. Roentgenographic patterns of Pneumocystis carinii pneumonia in 104 patients with AIDS. Chest. 1987;91(3):323-327. doi: 10.1378/chest.91.3.323
- Opravil M, Marincek B, Fuchs WA, et al. Shortcomings of chest radiography in detecting Pneumocystis carinii pneumonia. J Acquir Immune Defic Syndr.1994;7(1):39-45.
- Sax PE. Treatment and prevention of Pneumocystis infection in HIV-Infected patients. In: Barlett JG, Mitty J, eds. UpToDate. Waltham, MA: UpToDate Inc. uptodate.com/contents/treatment-and-prevention-of-pneumocystis-infection-in-hiv-infected-patients?search=pjp%20pneumonia%20treatment&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H494481841. Updated April 27, 2018.
- National Institutes of Health. Consensus statement on the use of corticosteroids as adjunctive therapy for Pneumocystis pneumonia in the acquired immunodeficiency syndrome. N Engl J Med. 1990;323(21);1500-1504. doi: 10.1056/NEJM199011223232131