Perianal Abscess
History of present illness:
31-year-old male with history of human immunodeficiency virus (HIV) presented with complaints of pain and redness to the right inner buttock; vital signs were within normal limits. On exam, he had an 8 cm x 2.5 cm area of induration, fluctuance, erythema, and tenderness to the right buttock along the gluteal cleft. There was no induration, tenderness, or purulent drainage noted on rectal exam.
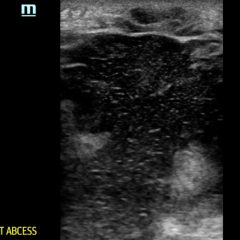
Significant findings:
Computed tomography (CT) of the Pelvis with intravenous (IV) contrast revealed a 5.7 cm x 2.4 cm air-fluid collection in the right perianal soft tissue along the right gluteal cleft, with surrounding fat stranding, consistent with a perianal abscess with cellulitis.
Discussion:
Perianal abscess typically presents as severe pain in the anorectal area that is constant and unrelated to bowel movement. Physical exam signs include perianal erythema with an associated palpable, often fluctuant, mass.1 However, physical examination may not adequately differentiate between a perianal abscess and perirectal abscess.2
A pelvic CT with IV contrast can be used to differentiate between a perianal abscess, which is located beneath the skin of the anal canal and does not transverse the external sphincter, and a perirectal abscess, which is located beyond the external anal sphincter. Ultrasound is emerging as a possible alternative imaging modality; however magnetic resonance imaging (MRI) and CT scans remain the modalities of choice. 3, 4, 5, 6
Recommended treatment for uncomplicated perianal abscesses is prompt drainage to avoid fistula formation, whereas complicated perirectal abscesses require a surgical consult.7 Patients younger than 40 and non-diabetics both have an increased risk (>2 and 2.69-fold, respectively) of fistula formation and chronic perianal abscess.8 Antibiotics are recommended for patients at risk of future infection, but have not been shown to reduce the incidence of fistula formation.9
Topics:
Perianal abscess, colorectal, Crohn’s disease, gastrointestinal, perirectal abscess.
References:
- Rizzo JA, Naig AL, Johnson EK. Anorectal abscess and fistula-in-ano: evidence-based management. Surg Clin North Am. 2010;90(1):45-68. doi: 10.1016/j.suc.2009.10.001
- Steele SR, Kumar R, Feingold DL, Rafferty JL, Buie WD. Practice parameters for the management of perianal abscess and fistula-in-ano. Dis Colon Rectum. 2011; 54(12):1465-1474. doi: 10.1097/dcr.0b013e31823122b3
- Schratter-Sehn AU, Lochs H, Vogelsang H, Schurawitzki H, Herold C, Schratter M. Endoscopic ultrasonography versus computed tomography in the differential diagnosis of perianorectal complications in Crohn’s disease. Endoscopy. 1993;25(09):582-586. doi: 10.1055/s-2007-1010409
- Domkundwar SV, Shinagare AB. Role of transcutaneous perianal ultrasonography in evaluation of fistulas In ano. J Ultrasound Med. 2007;26(1):29-36. doi: 10.7863/jum.2007.26.1.29
- Buchanan GN, Halligan S, Bartram CI, Williams AB, Tarroni D, Cohen CRG. Clinical examination, endosonography, and MR imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology. 2004;233(3):674-681. doi: 10.1148/radiol.2333031724
- Liang C, Lu Y, Zhao B, Du Y, Wang C, Jiang W. Imaging of anal fistulas: comparison of computed tomographic fistulography and magnetic resonance imaging. Korean J Radiol. 2014;15(6):712. doi: 10.3348/kjr.2014.15.6.712
- Berg DF, Bahadursingh AM, Kaminski DL, Longo WE. Acute surgical emergencies in inflammatory bowel disease. Am J Surg. 2002;184(1):45-51. doi: 10.1016/s0002-9610(02)00879-6
- Hamadani A, Haigh PI, Liu I-LA, Abbas MA. Who is at risk for developing chronic anal fistula or recurrent anal sepsis after initial perianal abscess? Dis Colon Rectum. 2009;52(2):217-221. doi: 10.1007/dcr.0b013e31819a5c52
- Sözener U, Gedik E, Kessaf Aslar A, Ergun H, Halil Elhan A, Memikoglu O, et al. Does adjuvant antibiotic treatment after drainage of anorectal abscess prevent development of anal fistulas? A randomized, placebo-controlled, double-blind, multicenter study. Dis Colon Rectum. 2011;54(8):923-929. doi: 10.1097/dcr.0b013e31821cc1f9