Pediatric Pulmonary Abscess
History of present illness:
A 6-year-old previously healthy male presented to the emergency department with three days of left upper quadrant abdominal pain. Family endorsed one week of fevers, cough productive of yellow sputum, and non-bilious, non-bloody emesis. He denied shortness of breath and chest pain. On exam, the patient was febrile with otherwise normal vital signs. He had diffuse tenderness to his abdomen but clear lungs. Laboratory studies revealed leukocytosis to 25,000/mm3 with a left shift.
Significant findings:
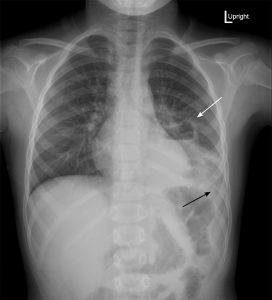
Upright posterior-anterior plain chest films show a left lower lobe consolidation with an air-fluid level and a single septation consistent with a pulmonary abscess (white arrows). A small left pleural effusion was also present, seen as blunting of the left costophrenic angle and obscuration of the left hemidiaphragm (black arrows).
Discussion:
Pediatric pulmonary abscesses are rare, most commonly caused by aspiration, and the majority consequently arise in dependent portions of the lung.1 The most common pathogens in children are Streptococcus pneumoniaeand Staphylococcus aureus.1 Immunocompromised patients and those with existing pulmonary disease more commonly contract Pseudomonas aeruginosaor Bacteroides, and fungal pathogens are possible.1 Common symptoms include tachypnea, fever, and cough. Imaging is necessary to distinguish pulmonary abscesses from pneumonia, empyema, pneumatocele, and other etiologies.
Plain film radiography may miss up to 18% of pulmonary abscesses yet is often the first modality to visualize an intrathoracic abnormality.2 If seen, pulmonary abscesses most often appear as consolidations with air-fluid levels. Generally, pulmonary abscesses are round with irregular, thick walls, whereas empyemas are elliptical with smooth, thin walls.3 However, these characteristics cannot definitively distinguish these processes.2 Advantages of plain films include being low cost and easily obtained. Computed tomography (CT) of the chest with contrast has 100% sensitivity for pulmonary abscess and empyema but is more expensive and less frequently available.
Most patients require admission and parenteral antibiotics covering Staphylococcus, Streptococcus, anaerobes, gram-negative bacilli, and in selected cases, Pseudomonas. Combined ceftriaxone and clindamycin is generally effective.1,5,6 With treatment, mortality is less than 5%, significantly better than for adults.1
Topics:
Pulmonary abscess, pediatrics, radiograph, air-fluid level, infection, empyema, lung.
References:
- Patradoon-Ho P, Fitzgerald DA. Lung abscess in children. Paediatr Respir Rev. 2007;8(1):77-84. doi: 10.1016/j.prrv.2006.10.002
- Stark DD, Federle MP, Goodman PC, Podrasky AE, Webb WR. Differentiating lung abscess and empyema: radiography and computed tomography. AJR Am J Roentgenol.1983;141(1):163-167. doi: 10.2214/ajr.141.1.163.
- Walker CM, Abbott GF, Greene RE, Shepard JO, Vummidi D, Digumarthy SR. Imaging pulmonary infection: classic signs and patterns. AJR Am J Roentgenol. 2014;202(3):479-492. doi: 10.2214/AJR.13.11463
- Groskin SA, Panicek DM, Ewing DK, Rivera F, Math K, Teixeira J, et al. Bacterial lung abscess: a review of the radiographic and clinical features of 50 cases. J Thorac Imaging. 1991;6(3):62-67. doi: 10.1097/00005382-199107000-00008
- Puligandla PS, Laberge JM. Respiratory infections: pneumonia, lung abscess, and empyema. Sem Pediatr Surg. 2008;17(1):42-52. doi: 10.1053/j.sempedsurg.2007.10.007
- Tan TQ, Seilheimer DK, Kaplan SL. Pediatric lung abscess: clinical management and outcome. Pediat Infect Dis J. 1995;14(1):51-55. doi: 10.1097/00006454-199501000-00011