Clinical Evaluation and Management of Pediatric Pericarditis
History of present illness:
A previously healthy 14-year-old male presented to the emergency department with complaints of chest tightness and pressure for the past two days. He noted shortness of breath and worsening of symptoms on the day of presentation. He denied fevers, myalgia, upper respiratory symptoms, or recent travel. The physical exam was unremarkable with normal heart sounds, no murmurs, rubs or gallops, and no chest wall tenderness to palpation. The patient’s chest X-ray was normal.
Significant findings:
An electrocardiogram (ECG) was concerning for ST segment elevation in leads II, III, aVF, and V4, with subtle ST elevations in V5 and V6 (see black arrows). There is also ST segment depression in aVL (see blue arrows).
Discussion:
The patient was found to have a troponin of 4 ng/mL. Pediatric cardiology was consulted in the emergency department, and an echocardiogram was performed which was within normal limits. The patient received non-steroidal anti-inflammatories in the emergency department and was discharged on ibuprofen with a diagnosis of acute pericarditis. Pediatric cardiology provided close follow-up including 48-hour, 2-week, and 6-week echocardiograms. Repeat echocardiograms were all normal, and the patient did well with resolution of his chest pain.
Pediatric pericarditis is a rare diagnosis in the emergency department. It accounts for less than 0.2% of pediatric chest pain visits.1 The clinical presentation typically includes chest pain, fever, tachycardia, and shortness of breath.2 The most common causes of pediatric pericarditis include viral or idiopathic etiology.2 On cardiac exam, the patient may have a high-pitched pericardial friction rub, although this finding is transient and varied between patient cases, with poor sensitivity (35%).3 However, when it is present, a pericardial friction rub has high specificity (approaching 100%) for acute pericarditis.4
Classic ECG findings include diffuse ST segment elevation, such as that seen in our patient, which is present in 65% to 70% of cases.3,5 PR-segment depression can be observed within the first hours to days, with ST segment depression in leads aVR and V1.6 Elevated inflammatory markers are often present.1,2 Elevated troponin levels are less common in acute pericarditis but one study reported they occurred in 32.2% of cases.3
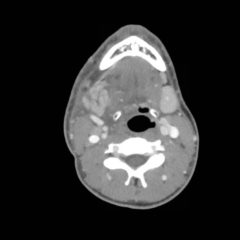
Echocardiograms are the optimal diagnostic tool, allowing for direct and noninvasive evaluation of the patient’s ejection fraction, with the ability to identify the presence of pericardial effusion.2 In thepediatric population, 37% to 68% of admissions for pericardial effusion occur as a result of idiopathic pericarditis.7 Serial echocardiograms can be used for follow up of stable patients. lternative imaging such as cardiac magnetic resonance imaging (CMR) or cardiac computed tomography (CT) may also be used for evaluation of injury.1 In a study evaluating the accuracy of CT findings in acute pericarditis, the sensitivity was 54%-59% with specificity of 91%-96%.8 CMR is the most sensitive method in diagnosing acute pericarditis, where regions of delayed gadolinium enhancement of the pericardium indicate inflammation and injury. It can be useful in cases where the diagnosis of pericarditis remains uncertain.6 Although CT and CMR studies may be performed, echocardiography remains the principal diagnostic method in the clinical evaluation of pericarditis.6
First-line management encompasses implementation of nonsteroidal anti-inflammatory therapy. This is often in combination with other anti-inflammatory medications such as corticosteroids, aspirin, colchicine, or methotrexate.7 Complications include the spread of inflammation within pericardial layers leading to involvement of the myocardium causing decreased left ventricular systolic function.9
Topics:
Chest pain, pediatric pericarditis, ECG, ST-segment elevation, echocardiogram, non-steroidal anti-inflammatory therapy.
References:
- Baskar S. Pediatric pericarditis. American College of Cardiology. http://www.acc.org/latest-in-cardiology/articles/2016/06/08/11/43/pediatric-pericarditis. Published June 8, 2016. Accessed September 27, 2018.
- Jone P, Darst JR, Collins KK, Miyamoto SD. Cardiovascular diseases. In: Hay WW, Jr., Levin MJ, Deterding RR, Abzug MJ, eds. CURRENT Diagnosis & Treatment Pediatrics. 24th ed. New York, NY: McGraw-Hill; 2018:604-605.
- Bainey KR, Bhatt DL. Acute pericarditis: appendicitis of the heart? Mayo Clin Proc. 2009;84(1):5-6.
- Tingle LE, Molina D, Calvert CW. Acute pericarditis. Am Fam Physician. 2007;76(10):1509-1514.
- Bonnefoy E, Godon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21(10):832-836. doi:1053/euhj.1999.1907
- Khandaker MH, Espinosa RE, Nishimura RA, Sinak LJ, Hayes SN, Melduni RM, et al. Pericardial disease: diagnosis and management. Mayo Clin Proc. 2010;85(6):572-593. doi: 10.4065/mcp.2010.0046
- Shakti D, Hehn R, Gauvreau K, Sundel RP, Newburger JW. Idiopathic pericarditis and pericardial effusion in children: contemporary epidemiology and management. J Am Heart Assoc. 2014;3: e001483. doi: 10.1161/jaha.114.001483
- Hammer MM, Raptis CA, Javidan-Nejad C, Bhalla S. Accuracy of computed tomography findings in acute pericarditis. Acta Radiologica. 2014;55(10):1197-1202. https://doi.org/10.1177/0284185113515866
- Cremer PC, Kumar A, Kontzias A, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol. 2016;68(21):2311-2328. doi: 10.1016/j.jacc.2016.07.785