Don’t Forget the Pacemaker – A Rare Complication
History of present illness:
An 85-year-old male with past medical history significant for atrial fibrillation complicated by sick sinus syndrome treated with pacemaker presents to the emergency department (ED) with a five-day history of weakness, intermittent lightheadedness, mild dyspnea on exertion, and intermittent diarrhea.
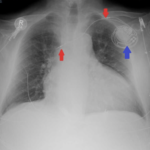
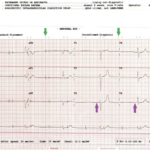
The patient’s chief complaint as documented by the triage nurse was “abdominal pain.” An electrocardiogram (ECG) order was automatically triggered by the ED electronic medical record system due to his age and chief complaint. The vital signs obtained in triage demonstrated a pulse in the 30’s and a systolic blood pressure in the low 100’s. The ECG was reviewed by the resident and attending physician, and he was placed on an external pacer. A portable chest X-ray was ordered.
Significant findings:
The ECG demonstrated the presence of pacemaker spikes without appropriate capture (green arrows) and a ventricular escape rhythm which can be identified by an absence of P waves prior to the QRS complex (purple arrows). The portable chest X- demonstrated displaced pacemaker leads (red arrows) that were coiled around the pulse generator (blue arrow).
Discussion:
Initially the patient adamantly denied that he ever touched his pacemaker site. However, his wife reported that the patient “always” touches the site. Electrophysiology was consulted, and he was started on a dopamine drip that resulted in an increase in heart rate. He was subsequently taken to the electrophysiology lab, where a small, wireless pacemaker device was placed.
This case demonstrates Reel syndrome, a variant of Twiddler’s syndrome, which occurs as the result of pacemaker malfunction secondary to patients’ manipulation of their pacemakers with lead retraction.1 Twiddler’s syndrome was first described in 1968.2 This complication of pacemaker placement occurs when a patient manipulates the pulse generator of his or her pacemaker so that the leads coil around the long access of the pulse generator. This type of manipulation usually results in lead fracture and the ECG will usually demonstrate complete pacing failure.3,4 Reel syndrome, as presented in this case, was first described in 1999.3 This pacemaker complication occurs when a patient “spins” his or her pacemaker along the transverse access of the pulse generator, which also results in lead coiling but usually does not result in lead fracture.3 The ECG in Reel syndrome can continue to demonstrate some pacing capture, depending on where the leads are located.
Elderly and obese patients tend to have looser subcutaneous tissue in the pacemaker pulse generator pocket, which makes movement of the device easier. Females, patients with dementia, and those with psychiatric disorders are also at an increased risk due to the tendency of these patient populations to inadvertently manipulate the pulse generator.3, 4, 5
In other reported cases of Twiddler’s syndrome, patients have experienced diaphragmatic contraction due to phrenic nerve stimulation or arm twitching secondary to brachial plexus stimulation.5 Possible treatments for this syndrome include minimizing patient’s pulse generator pocket size, post-operative compression bands for patients to wear on their upper chest and shoulders, and tighter suturing of the pulse generator.3,4
Topics:
Cardiac dysrhythmia, pacemaker, Twiddler’s syndrome, cardiology.
References:
- Bali HK, Chattree KK, Bali SK, Chauhan HK, Shukla CP. A tale of early Reel syndrome caused by an over-enthusiastic masseuse. Indian Heart J. 2013;65(6): 703-704. doi: 10.1016/j.ihj.2013.10.005
- Bayliss CE, Beanlands DS, Baird RJ. The Pacemaker-Twiddler’s syndrome: a new complication of implantable transvenous pacemakers. Can Med Assoc J. 1968;99(8):371-373.
- Munawar M, Munawar DL, Basalamah F, Pambudi J. Reel syndrome: a variant form of Twiddler’s syndrome. J Arrhythmia. 2011;27(4):338-342. doi: 10.1016/S1880-4276(11)80036-0
- Mandal S, Pande A, Kahali D. A rare case of very early pacemaker Twiddler’s Syndrome. Heart Views. 2012;13(3):114-115. doi: 10.4103/1995-705X.102157
- Nicholson WJ, Tuohy KA, Tikemeier P. Twiddler’syndrome. N Engl J Med.2003;348:1726-1727. doi: 10.1056/NEJM200304243481722