Erythema Migrans
History of present illness:
A 28-year-old male presented to the emergency department with a chief complaint of two weeks of headache, chills, and numbness in his hands. He reported removing a tick from his upper back approximately two weeks ago, but did not know how long the tick had been embedded. His review of symptoms was otherwise unremarkable.
Significant findings:
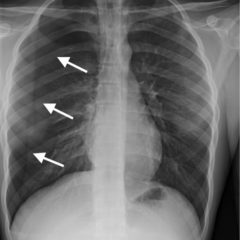
On physical examination, an 8-cm non-raised, erythematous lesion with central clearing was noted on the right posterior thorax. A small scab was located at the center of the lesion with no evidence of retained tick. No other rashes were present.
Discussion:
Lyme disease is a tick-borne illness caused primarily by the spirochete Borrelia burgdorferi. Ticks must be attached for a minimum of 48 hours in order to transmit the spirochete.1 Erythema migrans (EM) is the most common clinical manifestation of Lyme disease. EM is characterized by a slowly-expanding erythematous rash at the site of the tick bite, typically appearing between 7- and 14-days following tick attachment. Rashes range from 5cm to 30cm and may develop central clearing.2 Erythema migrans must be differentiated from initial erythema at the site of the bite due to a reaction to tick saliva. The differential includes southern tick-associated rash illness, erythema multiforme, cellulitis, contact dermatitis, and tinea corporis. The presence of erythema migrans has a sensitivity of 69% and a specificity of 98% for Lyme disease.3 Serological testing is not indicated in patients with EM, as only about 30% will be seropositive at presentation.4 Treatment of early Lyme disease consists of doxycycline preferentially, or amoxicillin, or cefuroxime for 14 days.6 Recurrence of erythema migrans after a full course of antibiotics is most likely due to re-infection rather than relapse.7 Prognosis is excellent with antibiotic treatment; however, those in endemic areas are at high risk for re-infection.8
Topics:
Erythema migrans, Lyme disease, Borrelia burgdorferi, infectious disease.
References:
- Sood SK, Salzman MB, Johnson BJ, Happ CM, Feig K, Carmody L, et al. Duration of tick attachment as a predictor of the risk of Lyme disease in an area in which Lyme disease is endemic. J Infect Dis.1997;175(4):996-999.doi: 10.1086/514009
- Bratton RL, Whiteside JW, Hovan MJ, Engle RL, Edwards FD. Diagnosis and treatment of Lyme disease. Mayo Clin Proc.2008;83(5):566-571. doi: 10.4065/83.5.566
- Aguero-Rosenfeld ME, Wang G, Schwartz I, Wormser GP. Diagnosis of Lyme borreliosis. Clin Microbiol Rev. 2005;18(3):484-509. doi: 10.1128/CMR.18.3.484-509.2005
- Nadelman RB, Nowakowski J, Forseter G, Goldberg NS, BIttker S, Cooper D, et al. The clinical spectrum of early Lyme borreliosis in patients with culture-confirmed erythema migrans. Am J Med.1996;100:502.
- Steere AC, McHugh G, Damle N, Sikand VK. Prospective study of serologic tests for Lyme disease. Clin Infect Dis.2008; 47(2):188-195. doi: 10.1086/589242
- Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, et al. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis.2006;43(9):1089-1134. doi: 10.1086/508667
- Nadelman, RB, Hanincova K, Mukherjee P, Liveris D, Nowakowski J, McKenna D, et al. Differentiation of reinfection from relapse in recurrent Lyme disease. N Engl J Med. 2012;367(20):1883-1890. doi: 10.1056/NEJMoa1114362
- Nowakowski, J, Nadelman RB, Sell R, McKenna D, Cavaliere LF, Holmgren D, et al. Long-term follow-up of patients with culture-confirmed Lyme disease. Am J Med. 2003;115(2)91-96.